Research Article
Thirty days post-operative complications after Sleeve Gastrectomy, Gastric Bypass and Mini Gastric Bypass/one Anastomosis Gastric Bypass. Analysis of the Italian Society for Bariatric Surgery and Metabolic Disorders (S.I.C.OB.) database of 7 years time frame

Maurizio De Luca1*, Nicola Clemente1, Cristiana Visentin2, Natale Pellicanò1, Cesare Lunardi1, Alberto Sartori1, Gianni Segato3, Luigi Angrisani4, Marcello Lucchese5 and Nicola Di Lorenzo6
1Department of General Surgery, Montebelluna Treviso Hospital, Italy
2Department of Statistics at Aulss n.8 Asolo Treviso, Italy
3Department of Surgery, Vicenza Regional Hospital, Italy
4University “Federico II” of Naples, Italy
5Department of Surgery, Santa Maria Nuova Hospital, Firenze, Italy
6Department of Surgery, Tor Vergata University, Rome, Italy
*Address for Correspondence: Maurizio De Luca, Department of General Surgery, Montebelluna Treviso Hospital, Italy, Tel: 338 9449298; Email: [email protected]
Dates: Submitted: 14 October 2017; Approved: 23 October 2017; Published: 24 October 2017
How to cite this article: De Luca M, Clemente N, Visentin C, Pellicanò N, Lunardi C, et al. Thirty days post-operative complications after Sleeve Gastrectomy, Gastric Bypass and Mini Gastric Bypass/one Anastomosis Gastric Bypass. Analysis of the Italian Society for Bariatric Surgery and Metabolic Disorders (S.I.C.OB.) database of 7 years time frame. Arch Surg Clin Res. 2017; 1: 062-071.
DOI: 10.29328/journal.ascr.1001011
Copyright License: © 2017 De Luca M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Clavidien-Dindo classification; Early complications; Sleeve gastrectomy; Roux-en-Y Gastric Bypass; Mini Gastric Bypass; S.I.C.OB. database
Abstract
Background: To date, the scientific community has mainly focused on outcomes of obesity surgery such as weight loss and resolution of associated complications. Adverse post-operative events and reoperation rates have been poorly reported even if they are a marker of surgical safety and therefore of great importance in guiding patients and surgeons in the choice of the more suitable operation.
Methods: This retrospective multicenter observational study is based on the data extracted from the Italian Society of Bariatric Surgery and Metabolic Disorders (S.I.C.OB.) database, which covers almost all the bariatric operations performed in Italy. We analysed the 30 days post-operative complications occurring, in the period from 2009 to 2015, after Roux-en-Y Gastric Bypass (RYGB), Sleeve Gastrectomy (SG) and Mini Gastric Bypass/One Anastomosis Gastric Bypass (MGB/OAGB) qualitatively, quantitatively and on the basis of the Clavien-Dindo classification of surgical complications. Complications following surgeries were tested using the 95% confidence interval. Statistical analysis was performed with Statistical Analysis System (SAS).
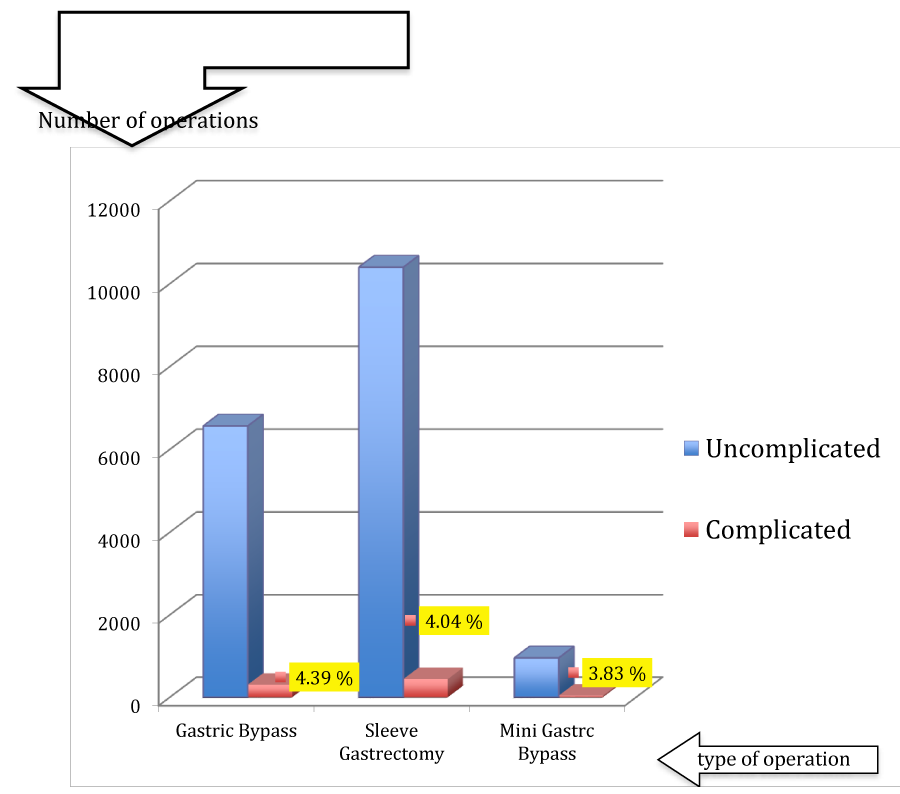
Results: In the 2009-2015 time frame, a total of 31,624 operations were performed of which 6,864 RYGB, 10,833 SG and 992 MGB/OAGB. The complication rate was 4.39 %, 4.04 % and 3.83% respectively. The most frequent complications were hemoperitoneum (0.9%) and perforation, fistula and dehiscence (1%) which were higher in SG when compared with RYGB (with a statistical significance) and when compared with MGB/OAGB (without a statistical significance). When dividing the complications by the different grades of the Clavien-Dindo classification, the only significant difference encountered, from a statistical standpoint, was between MGB/OAGB and SG. MGB/OAGB was associated with a lower grade I Clavien-Dindo complication rate (1.31% versus 2.34%).
Conclusion: This study supports a safe profile of obesity surgey in Italy, along with positive bariatric outcomes. The rate of 30 days post-operative complications is progressively lower after MGB/OAGB (3.83%), SG (4.04%) and RYGB (4.39%) respectively. In particular, MGB/OAGB records statistically less low-grade Clavien-Dindo complications compared to SG and RYGB.
Introduction
To date the scientific debate in the field of obesity surgery has mainly focused on weight loss and resolution of obesity associated comorbidities. Comparisons between different operations have been carried out in order to outline the one with the best outcomes. Adverse post-operative events and reoperation rates have been poorly reported.
Nevertheless these are a marker of surgical safety. An exact assessment of surgical safety is constantly required by patients, payers and health care providers. Moreover, an exact knowledge of the complication profile is crucial to improve surgical performance and decrease morbidity and mortality rates.
To address this issue, we carried out an analysis of the the Italian Society of Bariatric Surgery and Metabolic Disorders (S.I.C.OB.) database which covers almost all the bariatric operations performed in Italy. We restricted our attention to the 7 years period from 2009 to 2015 and to three major operations namely Roux-en Y Gastric Bypass (RYGB), Sleeve Gastrectomy (SG) and Mini Gastric Bypass/One Anastomosis Gastric Bypass (MGB/OAGB). Early post-operative complications occurring after these surgeries were analysed qualitatively, quantitatively and on the basis of the Clavien-Dindo classification of surgical complications.
Materials and Methods
The present retrospective multicenter observational study is based on data extracted from the S.I.C.OB. database. This is a registry based on prospectively collected data from 121 participating Centers located all over Italy. S.I.C.OB. Registry dates back to 1990, followed by transition to the online version in 2007. The S.I.C.OB. database covers almost all the bariatric operations performed to date within the the national ZDFSVVVXVs. It consists of three distinct sections. 1) The first one collects demographic data such as gender (male or female), date of birth, geographical origin (North Italy, Central Italy, South Italy or major islands), smoking habit, previous bariatric surgery. 2) The second contains the “peri operative” data; specifically, the pre-operative ones are type, date, duration of operation. Surgical access (open versus laparoscopic) and conversion from one to another is also reported; so are technical details, specific of each operation (eg. volume of gastric pouch and/or use of a calibration bougie in case of surgeries involving gastric restriction; length of intestinal limbs in case of intestine diversions; use of methylene blu die leakage-test in construction of anastomoses are part of the operation). The post-operative data include ICU stay, date of hospital discharge, type of complication (if any) and its treatment (none, pharmacological treatment, mini invasive interventions, surgical intervention with or without intermediate care/ICU management). 3) The third section of the S.I.C.OB. database contains the follow-up data. These are weight loss, excess weight loss, resolution of associated comorbidities (eg. diabetes, hypertension, dyslipidemia, obstructive sleep apnea syndrome), restoration of normal anatomy and the reason for it, switch to another operation and indication to it, long-term postoperative complications (eg. dysphagia and vomiting, anemia, lithiasis, incisional hernia, micronutrient deficiencies, oesophagitis, gastritis), death and cause of death. To make evaluation of results easier, this third section includes some pre-operative antropometric parameters such as height, initial weight, body mass index, dietary habits (nibbling, binge eating, sweet eating) and associated comorbidities.
Data, within each section, are collected anonymously but a univocal identification code enables to link together data regarding the same patient and make analyses possible. Two independent statisticians were involved in the extraction and analysis of data. As an initial step, the time frame of the analysis was restricted to the 7 years period ranging from Jan 2009 to Dec 2015. Then, only data regarding RYGB, SG and MGB/OAGB were retrieved. In particular, to the aim of our study, variables of interest were the early (30 days) post-operative complications after the above mentioned interventions. These variables are rated within the S.I.C.OB. database as discrete variables (presence or absence of a specific complication). Similarly, the degree of severity of each complication is rated as a quantitative discrete variable as it ranges from grade I to grade V according the Clavien-Dindo classification. Given the quantitative discrete nature of the variables, the statistics used for our comparative analysis were proportions (ratio between the number of complications and the total number of operations, number of complication of a specific Clavien-Dindo grade out of the total number of the operations in examination) and the relative confidence interval at the 95° percentile. Complications following surgeries were tested using the 95% confidence interval. Statistical analysis was performed with Statistical Analysis System (SAS).
No ethical approval was required for this retrospective study as it was based on anonymized data.
Results
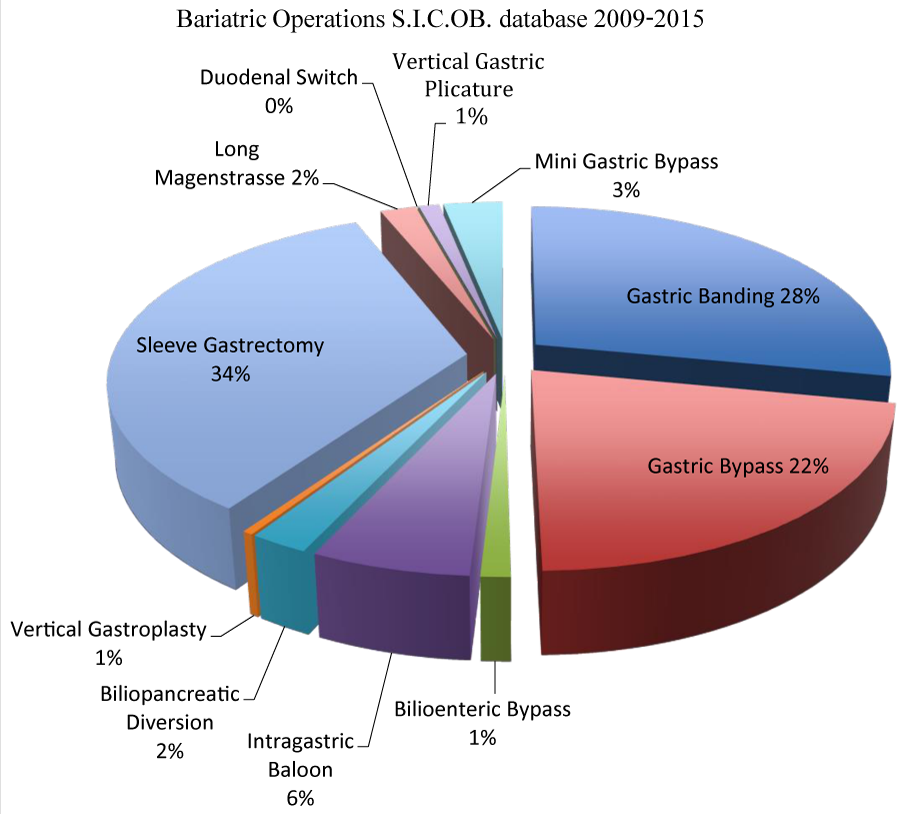
In the 2009-2015 time frame, a total of 31,624 operations were performed of which 8,875 Gastric Banding (GB) 6,864 RYGB, 359 Bilio-Enteric Bypass (BEB), 1,918 Intragastric Balloon (IB), 710 BilioPancreatic Diversion (BPD), 126 Vertical Gastroplasty (VBG), 10,833 SG, 604 Long Magenstrasse (LM), 2 Duodenal Switch (DS), 341 Vertical Gastric Plicature (VGP), 992 MGB/OAGB.
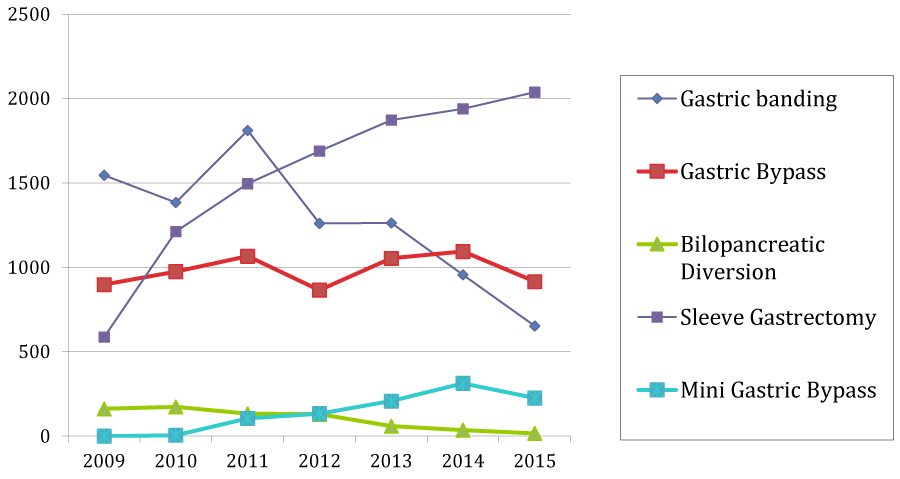
The most commonly performed operations were SG (34%), GB (28%) and RYGB (22%). The least performed were BPD (approx 1%) and DS (approx 0%). There was a trend toward a reduction of the GB over these years maybe as a consequence of the multiple studies reporting on re-operations following this surgery. On the other hand, SG has progressively gained popularity being the most frequently performed bariatric operation to date. About 34% of all the operations reported on the S.I.C.OB. database from 2009 to 2015 are represented by SG. It has been proved to be technically simple for the surgeon, efficacious with regard to weight loss and when not efficacious easily convertible into a second operation.
RYGB was performed with an almost unchanged frequency over the years in scrutiny. The slight decrease which can be detected in last two years is in parallel with the increase of another mainly restrictive-malabsorptive operation known as MGB/OAGB. MGB/OAGB seems to be equally effective to RYGB in reducing weight but less technically demanding. Introduced by Rutledge [1], it represents no more than 3% of all the operation registered in the S.I.C.OB. database.
BPD is among the least adopted operation with no detectable variation in frequency over the years. Technical complexity and serious side effects makes this operation, with both restrictive and malabsoptive mechanism, indicated only in an highly selected group of patients (Figure 1).
Figure 1: S.I.C.OB. database: overview of all the bariatric operations performed during the period 2009-2015 with their relative percentage.
All this considered, we decided to restrict our investigation on the operations which presently are or are likely to become the most frequent ones: SG, RYGB and MGB/OAGB. In particular, we focused our analysis on the specific issue of 30 days (“early”) postoperative complications. This is undoubtably a matter of great importance because complications are a marker of surgical safety. Postoperative complications are recorded in the SICOB data base as “early postoperative complications” when occurring between operation and first follow-up visit which is usually scheduled within 30 days from discharge. So “early” can be considered synonymous with “30 days” complications. The overall early complication rate was 4.39 %, 4.04 % and 3.83 % for RYGB, SG and MGB/OAGB respectively (Figure 2).
Figure 2: S.I.C.OB. database: changing frequency of adoption over time of Gastric Banding, Gastric Bypass, BilioPancreatic Diversion, Sleeve Gastrectomy and Mini Gastric Bypass.
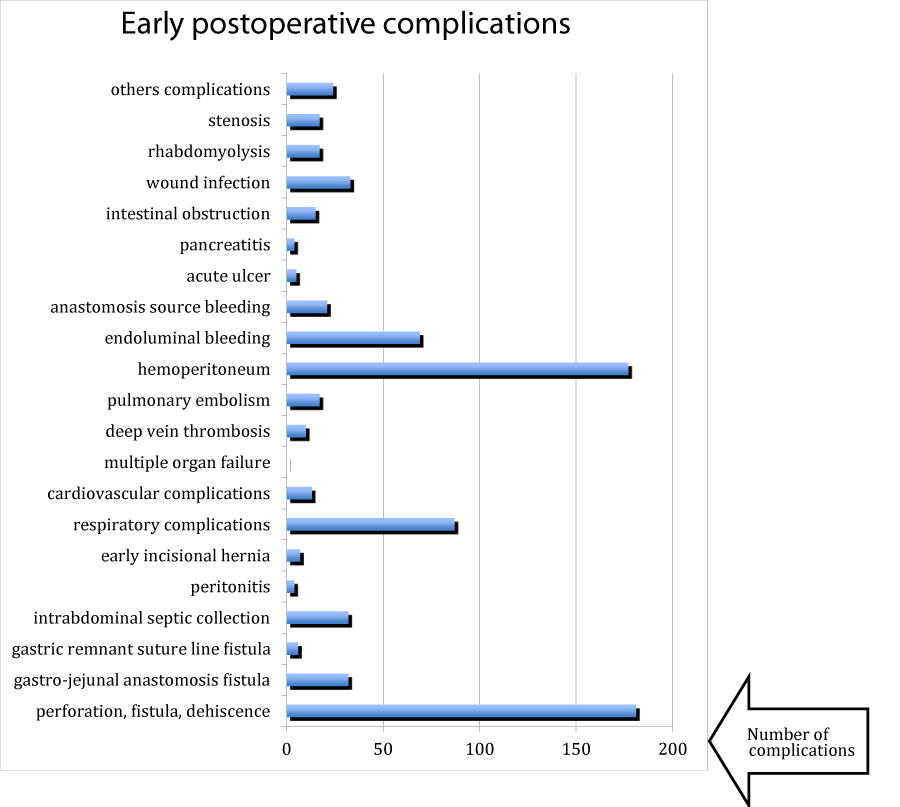
The array of complications reported is extremely wide and consists of perforation, dehiscence, gastro-jejunal anastomosis fistula, gastric remnant suture line fistula, total perforation/fistula/dehiscence, intrabdominal septic collection, peritonitis, early incisional hernia, respiratory complications, cardiovascular complications, multiple organ failure, deep venous thrombosis, pulmonary embolism, hemoperitoneum, endoluminal bleeding, anastomosis-source bleeding, acute ulcer, pancreatitis, intestinal obstruction, wound infection, rhabdomyolysis, stenosis, others.
The most frequent complications were hemoperitoneum (0.9%) and perforation, fistula and dehiscence (1%) (Figure 3). A comparative analysis of the proportions and their relative confidence intervale at 95° percentile between the three operations under scrutiny was carried out (Table 1). The only significative difference, from a statistical point of view, was an higher proportion of post operative hemoperitoneum after SG in comparison with RYGB (1.3% versus 0.4% respectively). Despite a quite similar difference in the respective proportions, the same didn’t hold true when comparing SG with MGB/OAGB (1.3% versus 0.6% respectively).
Figure 3: S.I.C.OB. database: comparison (absolute numbers on the y-axis; proportions in the labels) between uncomplicated and complicated operations of Roux-en Y Gastric Bypass, Sleeve Gastrectomy, and Mini Gastric Bypass in the 2009-2015 period.
| Table 1: S.I.C.OB. database: post-operative complications occurred after RYGB, SG, and MGB/OAGB expressed as absolute number, percentage and confidence interval at 95° percentile. | ||||
| Gastric Bypass n= 6,864 |
Sleeve Gastrectomy n= 10,833 |
Mini Bypass n = 992 |
total n= 18,689 |
|
| perforation, fistula, dehiscence | 44 0.6 (0.5-0.8) |
130 1.2 (1-1.4) |
7 0.7 (0.2-1.2) |
181 1 (0.8-1.1) |
| gastro-jejunal anastomosis fistula | 29 0.4 (0.3-0.6) |
0 | 3 0.3 (0.0-0.6) |
32 0.2 (0.1-0.2) |
| gastric remnant suture line fistula | 5 0.1 (0.0-0.1) |
0 | 1 0.1 (0.1-0.3) |
6 0 (0.0-0.1) |
| intra-abdominal septic collection | 9 0.1 (0.0-0.2) |
22 0.2 (0.1-0.3) |
1 0.1 (0.1-0.3) |
32 0.2 (0.1-0.2) |
| peritonitis | 1 0 (0.0-0.1) |
2 0 (0.0-0.1) |
0.0 (0.0-0.0) | 3 0 (0.0-0.1) |
| early incisional hernia | 7 0.1 (0.0-0.1) |
0.0 (0.0-0.0) | 0.0 (0.0-0.0) | 7 0 (0.0-0.1) |
| respiratory complications | 37 0.5 (0.4-0.7) |
44 0.4 (0.3-0.5) |
6 0.6 (0.1-1.1) |
87 0.5 (0.4-0.6) |
| cardiovascular complications | 4 0.1 (0.0-0.1) |
9 0.1 (0.0-0.1) |
0.0 (0.0-0.0) | 13 0.1 (0.0-0.1) |
| multiple organ failure | 0.0 (0.0-0.0) | 0.0 (0.0-0.0) | 0.0 (0.0-0.0) | 0 0 (0.0-0.0) |
| deep vein thrombosis | 2 0 (0.0-0.1) |
8 0.1 (0.0-0.1) |
0.0 (0.0-0.0) | 10 0.1 (0.0-0.1) |
| pulmonary embolism | 13 0.2 (0.1-0.3) |
3 0 (0.0-0.1) |
1 0.1 (0.1-0.3) |
17 0.1 (0.0-0.1) |
| hemoperitoneum | 28 0.4 (0.3-0.6) |
143 1.3 (1.0-1.5) |
6 0.6 (0.1-1.1) |
177 0.9 (0.8-1.0) |
| endoluminal bleeding | 37 0.5 (0.4-0.7) |
30 0.2 (0.1-0.3) |
2 0.2 (0.1-0.5) |
69 0.3 (0.2-0.4) |
| bleeding from anastomosis | 16 0.2 (0.1-0.3) |
0.0 (0.0-0.0) | 5 0.5 (0.1-0.9) |
21 0.1 (0.1-0.3) |
| acute ulcer | 5 0.1 (0.0-0.1) |
0.0 (0.0-0.0) | 0.0 (0.0-0.0) | 5 0 (0.0-0.1) |
| pancreatitis | 0.0 (0.0-0.0) | 4 0 (0.0-0.1) |
0.0 (0.0-0.0) | 4 0 (0.0-0.1) |
| intestinal obstruction | 13 0.2 (0.1-0.3) |
0.0 (0.0-0.0) | 2 0.2 (0.1-0.5) |
15 0.1 (0.0-0.1) |
| wound infection | 30 0.4 (0.3-0.6) |
13 0.1 (0.1-0.2) |
0.0 (0.0-0.0) | 33 0.2 (0.2-0.3) |
| rhabdomyolysis | 9 0.1 (0.0-0.2) |
4 0 (0.0-0.1) |
4 0.4 (0.0-0.8) |
17 0.1 (0.0-0.1) |
| stenosis | 5 0.1 (0.0-0.1) |
12 0.1 (0.0-0.2) |
0.0 (0.0-0.0) | 17 0.1 (0.0-0.1) |
| others | 8 0.1 (0.0-0.1) |
14 0.1 (0.0-0.1) |
0.0 (0.0-0.0) | 22 0.1 (0.0-0.1) |
| total complications | 302 | 438 | 38 | 778 |
Similarly, the “perforation, fistula and dehiscence” complications, as they are cumulatively reported in the S.I.C.OB. database, were statistically more frequent in SG rather than in RYGB (1.2 % versus 0.6% respectively). The 0.7% proportion of “perforation, fistula and dehiscence” in MGB/OAGB wasn’t statistically different from the 1.2% following SG.
Obviously, each of these complications can be of different severity and it is acknowledged that no proper interpretation of surgical outcome data can be drawn without taking into account the severity degree. For the purpose of our analysis, we used the Clavien-Dindo classification of surgical complications which is a 5-scale classification system introduced in 2004 by the eponymous Authors [2]. Since its pubblication, this classification proved to be an objective, simple, reliable, and reproducible way of reporting negative events after surgery and it was widely adopted in the scientific literature. This system ranks the complications by severity on the basis of the type of therapy required to treat the complication (Table 2).
| Table 2: The Clavien-Dindo classification of surgical complications. | |
| I | Any deviation from the normal postoperative course without pharmacologic treatment or surgical, endoscopic, and radiological interventions. Allowed therapeutic regimens are: drug as antiemetics, antipyretics, analgesics, diuretics, electrolytes, and physiotherapy. This grade also includes wound infections opened at the bedside. |
| II | Requiring pharmacologic treatment with drugs other than ones allowed for grade I complications. Blood transfusion and total parenteral nutrition are also included. |
| III -IIIa -IIIb |
Requiring surgical, endoscopic, or radiologic intervention: - Intervention not under general anesthesia; - Intervention under general anesthesia |
| IV -IVa -IVb |
Life-threatening complications (including central nervous system complications) requiring intermediate care/ICU management:
-Single-organ dysfunction (including dialysis); - Multiorgan dysfunction |
| V “d” suffix |
Death of a patient. If the patient suffers from a complication at the time of the discharge, the suffix “d” (for disability) is added to the respective grade of complication (including resection of the pancreatic remnant). This label indicates the need for a follow-up to fully eveluate the complication. |
Similarly, complications are reported into the S.I.C.OB. data base according this classification.
Using the Clavien-Dindo classification, 17,911 out of 18,689 (95,8%) patients had no complications. The overall postoperative mortality rate (grade V) was 0.15%. When dividing the complications by the different grades of the Clavien-Dindo classification, the only significant difference, from a statistical standpoint, was between MGB/OAGB and SG. The former was associated with a lower grade I complication rate (1.31% versus 2.34%). Though apparently similar, the difference in grade I complication rate between MGB/OAGB and RYGB (1.31% versus 2.30%) didn’t reach any statistical significance because of overlapping confidence intervals (Table 3).
| Table 3: Post-operative complications after RYGB, SG and MGB/OAGB according the Clavien-Dindo classification: number of complications, percentage and confidence interval at 95° percentile in each grade. | |||||||||
| Gastric Bypass | Sleeve Gastrectomy | Mini Gastric Bypass/One Anastomosis Gastric Bypass | |||||||
| Clavien-Dindo grade | number of complications | % | confidence interval | number of complications | % | confidence interval | number of complications | % | confidence interval |
| no complication | 6562 | 95.6% | 95.1-96.1 | 10395 | 95,9% | 95.6-96.3 | 954 | 96,1% | 95.0-97.4 |
| I | 158 | 2.30% | 1.9-2.7 | 254 | 2.34% | 2.1-2.6 | 13 | 1.31% | 0.6-2.0 |
| II | 94 | 1.36% | 1.1-1.6 | 120 | 1.10% | 0.9-1.3 | 18 | 1.81% | 1.0-2.6 |
| III | 14 | 0.20% | 0.1-0.3 | 14 | 0.12% | 0.1-0.2 | 3 | 0.30% | 0.0-0.6 |
| IV | 20 | 0.29% | 0.2-0.4 | 37 | 0.34% | 0.2-0.5 | 4 | 0.40% | 0.0-0.8 |
| V (death) | 16 | 0.23% | 0.1-0.3 | 13 | 0.12% | 0.1-0.2 | 0 | 0% | 0.0 |
| total | 6864 | 10833 | 992 | ||||||
Discussion
To date the scientific debate in the field of obesity surgery has mainly focused on outcomes of surgery such as weight loss and obesity associated comorbidities compared with non-surgical interventions. Comparisons between the different surgical procedure have also been carried out. As a result, it is unanimously accepted that bariatric surgery, regardless of the type of procedure used, results in better and longer-lasting weight loss and in greater improvement of comorbidities compared with non surgical operations [3]. When compared with each other, certain procedures results in greater weight loss and improvements in comorbidities than others. A Cochrane review [3], first published in 2003 and updated in 2014 analysed twenty-two Randomised Controlled Trials (RCTs) with 1798 participants. The outcomes considered, among the others, were excess weight loss and resolution of comorbidities. The conclusions drawn by the Authors were that RYGB and SG had similar outcomes, and both of these procedures had better outcomes than LAGB. This difference persisted over time. Indeed, SG was found to induce better weight-loss outcomes than LAGB still after three years of follow-up.
On the other hand, for people with very high BMI, DS resulted in greater weight loss than RYGB.
The results of this review are consistent with SG (34%) and RYGB (22%) being the most adopted operations in Italy according to the S.I.C.OB. database in the 2009-20015 period (Figure 4). LAGB, though still accounting for 28% of all the bariatric operations, showed a decreasing trend over the same time frame (Figure 1), when analysing the S.I.C.OB. database. The worse efficacy in meeting the goals of weight reduction and resolution of comorbidities is a valid explanation. Another one, is the recognition of the multiple short and long-term complications which make the risk-benefit ratio of LAGB rather unfavourable. This topic was highlighted by multiple studies. To name but a few, a recent multicenter, retrospective, matched cohort study conducted by Dogan et al. [4], in 2015 demonstrated that after 3 years of follow-up, LAGB showed a higher complication rate compared to SG and RYGB (p<0.05). Revisional surgery after LAGB was needed in 21%, while only 9% of the SG underwent conversion to RYGB. Himpens et al.[5], demonstrated that LAGB is associated with low perioperative morbidity but presents a failure rate between 20% and 30%, a late complication rate of 40.1% and a rate of reoperation of 20.4 %.
Figure 4: S.I.C.OB. database: different types of early post-operative complications reported after SG, RYGB and MGB/OAGB (absolute numbers on the x-axis).
Analysis of the S.I.C.OB. database in the 2009-2015 period, 7 years, showed that RYGB was performed with an almost unchanged frequency; only a slight decrease was detectable in last two years which was in parallel with the increase of another restrictive-malabsorptive operation, MGB/OAGB. Nowadays MGB/OAGB is progressively gaining great favour among bariatric surgeons as it seeems to be equally effective to RYGB in reducing weight but less technically demanding [6]. Because of its introduction in 1997 by Rutledge, the absolute number of this type of operation is still low. To date it represents no more than 3% of all the interventions reported into the S.I.C.OB. database. Nevertheless a rapid increase can be expected in the next years as positive results from RCT spanning 15-20 years will be accumulated.
BPD appears to be one of the least adopted operation (2% of all the bariatric procedures). Noteworthy, in the S.I.C.OB. database, only 2 cases are reported of the BPD-DS as variant of this operation. Their frequency over the 2009-2015 years didn’t show any significant fluctuation. Technical complexity and serious side effects makes these operations, with both restrictive and malabsoptive mechanism, indicated only in selected group of patients (Figure 1). Indeed, as suggested by the Cochrane review [3], BPD-DS is the operation of choice for people with very high BMI, no compliance to dietary restrictions or for nibblers and sweet eaters. In these patients it can result in greater weight loss than RYGB. The above mentioned Cochrane review points out another feature of extreme interest. Across all the studies considered, adverse event rates and reoperation rates were generally poorly reported.
That is a major drawback because an exact estimate of the complication rate is of crucial importance both for patients and health care providers. Indeed, post-operative complications are a marker of surgical safety. An exact assessment of surgical safety is constantly required by patients, payers and health care providers. Patients frequently ask for a precise quantification of the risks connected with the operation they are undertaking. Health care providers are committed to tailor the operation to the patient with respect to goals to be met (weight loss) and to the risk profile. More severe the grade of obesity and better the performance status of the patient, more aggressive and risky the operation could be. Conversely, worse the patient performance status, safer the complication profile of the operation should be.
Moreover, from a scientific standpoint, an evaluation of surgical safety on the basis of the post-operative complications is crucial to improve surgical performance and decreasing morbidity rates. Analysis of the S.I.C.OB. database, restricted to the 2009-2015 period, showed that 17,911 out of 18,689 (95.8%) patients who had either RYGB or SG or MGB/OAGB, had no complications. Within the same population and time frame, overall postoperative mortality rate was 0.15%. After subgroup analysis, we found a complication rate of 4.39 %, 4.04 % and 3.83 % for RYGB, SG and MGB/OAGB respectively. These data are consistent with those reported in other countries and support the safety of the operations under scrutiny [7-12]. The array of complications reported was extremely wide. The most frequent complications were hemoperitoneum (0.9%) and perforation, fistula and dehiscence (1%). These were the only complications whose frequency was significantly different between the operations under scrutiny. In particular, the proportion of post operative hemoperitoneum after SG was definitely higher than after RYGB (1.3% versus 0.4% respectively). The difference in frequency of hemoperitoneum between SG (1.3%) and MGB/OAGB (0.6%) was quite similarly though didn’t reach statistical weight. The very long section of the stomach, along with the division of the short gastric vessels, which are essential steps of SG, could explain the higher bleeding risk of this operation.
Similarly, the “perforation, fistula and dehiscence” complications, as they are cumulatively reported in the S.I.C.OB. database, were statistically more frequent in SG rather than in RYGB (1.2% versus 0.6% respectively). The 0.7% proportion of “perforation, fistula and dehiscence” in MGB/OAGB wasn’t statistically different from the 1.2% following SG. It is well acknowledged in the scientific community, that the sleeved stomach with an intact pylorus act as an high pressure cavity and this makes dehiscence of the stapled line and fistula much more likely to develop.
The rate of perioperative complications and mortality are only a rough estimation of the safety of the operation. The severity of complications is of equal, if not greater, relevance. The Clavien-Dindo classification, introduced in 2004 by the eponymous Authors allows to distinguish a normal postoperative course from any deviation from it. It ranks the severity of complications on the basis of the type of therapy required to treat the complication. The Clavien-Dindo system was validated through a large cohort of patients, who underwent a variety of surgical procedures and was also tested for its simplicity and “interobserver” variation in 10 centers around the world. Since its pubblication, this classification proved to be an objective, simple, reliable, and reproducible way of reporting negative events after surgery and it was widely adopted in the scientific literature. Similarly, it was adopted by the S.I.C.OB. database to report complications.
When dividing the complications by the different grades of the Clavien-Dindo classification, the only significant difference, from a statistical standpoint, was between MGB/OAGB and SG. The former was associated with a lower grade I complication rate (1.31% versus 2.34%). Though apparently similar, the difference in grade I complication rate between MGB/OAGB and RYGB (1.31% versus 2.30%) didn’t reach any statistical significance because of overlapping confidence intervals. Several Authors supporting this tecnique advocated a more favourable safety profile of this operation [6]. MGB/OAGB involves the creation of a sleeved gastric pouch along the lesser gastric curvature. The pouch is longer than that in traditional RYGB as it extends from the antrum, distal to the crow’s foot to esophago-gastric junction. A 1.5-3.0 cm wide, antecolic, antegastric Billroth II loop gastrojejunostomy is performed with a jejunal loop located at 150-250 cm from the Treitz ligament. Care is taken to position the proximal (or afferent) limb on the left side and the distal (or efferent) limb on the right side of the gastric pouch to avoid torsion. Moreover the side to side gastrojejunostomy brings the afferent limb at an higher level than the efferent one and this facilitates transit of food in the efferent rather than in biliopancreatic limb [6].
It was reported that the single gastro-jejunal anastomosis of MGB/OAGB makes this operation simpler and faster than RYGB. The subsequent shorter operative time could reduce complication linked with prolonged anaesthesia and immobilization (respiratory complications, deep vein thrombosis, pulmonary embolism, rhabdomyolisis). A lower incidence of internal herniation and abdominal pain was advocated because of the absence of mesenteric defect [11]. Moreover a reduced incidence of bleeding from anastomosis was deemed likely as only one anastomosis is performed rather than two. Noteworthy, bleeding from the gastrojejunostomy in MGB/OAGB could be more easily treated by mini invasive technique (upper endoscopy); the same didn’t hold true in case of bleeding from the jejuno-jejunostomy at Roux foot in RYGB. This should downgrade the severity of this possible complication from grade IV (surgical treatment) to grade III (mini invasive treatment).
These findings could not be verified by our analysis of the S.I.C.OB. database because none of the reported complications appeared to be statistically lower than the respective ones after SG and RYGB. This is probably the consequence of the small sample of the MGB/OAGB population (992 patients) in our study. Nevertheless a more favourable profile of this operation was evident as MGB/OAGB was associated with a statistically lower grade I complication rate (1.31%) when compared with SG (2.34%) and (though without any statistical significance) with RYGB (2.30%).
Conclusions
The current study is based on the analysis of data retrieved from the S.I.C.OB. database which covers almost all the bariatric operations performed in Italy. The early post-operative complications occurring after the RYGB, SG and MGB/OAGB, performed in the 2009-2015 time frame, were analysed qualitatively, quantitatively and on the basis of the Clavien-Dindo classification of surgical complications. Data for such analysis, from 2009 to 2015, were retrieved from the S.I.C.OB. database which covers almost all the bariatric operations carried out in Italy.This study supports a safe profile of obesity surgey in Italy, along with positive bariatric outcomes. The rate of 30 days post-operative complications is progressively lower after MGB/OAGB, SG and RYGB respectively. In particular, MGB/OAGB is associated with statistically less low-grade Clavidien-Dindo complications compared to SG and RYGB.
This study supports a safe profile of obesity surgey in Italy, along with positive bariatric outcomes. The rate of 30 days post-operative complications is progressively lower after MGB/OAGB, SG and RYGB respectively. In particular, MGB/OAGB is associated with statistically less low-grade Clavidien-Dindo complications compared to SG and RYGB.
Acknowledgments
This study has been written by a working group formed by members of Italian Society of Surgery for Obesity and Metabolic Disorders (SICOB) and has been discussed and approved by the Executive Board of the Italian Society of Surgery for Obesity and Metabolic Disorders (SICOB).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
References
- Rutledge R. The mini-gastric bypass: experience with the first 1274 cases. Obes Surg. 2001; 11: 276-280. Ref.: https://goo.gl/zMsvGU
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240: 205-213. Ref.: https://goo.gl/ZiGyxy
- Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014; 8. Ref.: https://goo.gl/XHMxZS
- Dogan K, Gadiot RP, Aarts EO, Betzel B, van Laarhoven CJ, et al. Effectiveness and Safety of Sleeve Gastrectomy, Gastric Bypass, and Adjustable Gastric Banding in Morbidly Obese Patients: a Multicenter, Retrospective, Matched Cohort Study. Obes Surg. 2015; 25: 1110-1118. Ref.: https://goo.gl/HsgC9K
- Himpens J, Dapri G, Cadiere GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg. 2006; 16: 1450-1456. Ref.: https://goo.gl/u8Jxy7
- Chevallier J M, Arman G, Guenzi M, Rau C, Bruzzi M, et al. One Thousand Single Anastomosis (Omega Loop) Gastric Bypasses to Treat Morbid Obesity in a 7-Year Period: Outcomes Show Few Complications and Good Efficacy. Obes Surg. 2015; 25: 951-958. Ref.: https://goo.gl/t1pq6Y
- Garofalo F, Denis R, Abouzahr O, Garneau P, Pescarus R, et al. Fully Ambulatory Laparoscopic Sleeve Gastrectomy: 328 Consecutive Patients in a Single Tertiary Bariatric Center. Obes Surg. 2015; 26: 1429-1435. Ref.: https://goo.gl/f5eTY6
- Clough A, Hamill D, Jackson S, Remilton M, Eyre R, et al. Outcome of three common bariatric procedures in the public sector. ANZ J Surg. 2016. Ref.: https://goo.gl/BfLCS7
- Georgiadou D, Sergentanis TN, Diamantis T, Tsigris C, Psaltopoulou T, et al. Efficacy and safety of laparoscopic mini gastric bypass. A systematic review. Surg Obes Relat Dis. 2014; 10: 984-991. Ref.: https://goo.gl/HQJRgJ
- Falk V, Twells L, Gregory D, Murphy R, Smith C, et al. Laparoscopic sleeve gastrectomy at a new bariatric surgery centre in Canada: 30-day complication rates using the Clavien-Dindo classification. Can J Surg. 2016; 59: 93-97. Ref.: https://goo.gl/i7bZSn
- Rojhani-Shirazi Z, Amini M, Meftahi N, Seperhrimesh M, Poorbaghi SL, et al. Comparison of aanthropometric measures in people with and without short-and long-term complications after laparoscopic sleeve gastrectomy. Comparative Clinical Pathology. 2017: 26: 1375-1379. Ref.: https://goo.gl/qyHn4a
- Amini M, Vafa L, Poorbaghi SL, Seperhrimesh M. Obesity and Weight Loss Therapy. J Obesity and Weight Loss Therapy. 2016; 6: 4.
- Peraglie C. Laparoscopic mini-gastric bypass (LMGB) in the super-super obese: outcomes in 16 patients. Obes Surg. 2008; 18: 1126-1129. Ref.: https://goo.gl/sgfvu7