More Information
Submitted: 10 October 2020 | Approved: 29 October 2020 | Published: 31 October 2020
How to cite this article: Şen DÖ, Irız B, Atay ÜT, Öncü E. Intentıonal reımplantatıon of hopeless teeth: Cases serıes. Arch Surg Clin Res. 2020; 4: 047-050.
DOI: 10.29328/journal.ascr.1001053
Copyright License: © Şen DÖ, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Intentıonal reımplantatıon of hopeless teeth: Cases serıes
Dilek Özkan Şen, Betül Irız, Ümmühan Tekin Atay and Elif Öncü*
Necmettin Erbakan University Faculty of Dentistry Departmant of Periodontolgy, Konya, Turkey
*Address for Correspondence: Elif Öncü, Necmettin Erbakan University Faculty of Dentistry Departmant of Periodontolgy, Konya, Turkey, Tel: +90 332 2200025; Fax: +90 332 2200026; Email: [email protected]; [email protected]
Intentional replantation is an alternative for the treatment of advanced periodontal destruction of the anterior teeth. Systemically healthy three female patient was referred to our clinic with functional complaints. Diagnosis were chronic periodontitis and class III mobility was noted at the mandibular incisors with complete periodontal attachment loss. After phase I periodontal treatment periodontally involved teeth were extracted, endodontic treatment accomplished, the teeth were replanted and fixed to its place with fiber reinforced composite splint. At the end of 2 years tooth was in function with alveolar bone gain. Intentional replantation provided long-term maintenance of patient’s own teeth.
The main purpose of periodontal therapy is the restoration of tissues lost due to periodontal disease [1]. There are many biological and functional challenges in the management of anterior teeth manifesting excessive periodontal destruction. Both surgical and non-surgical methods are not successful, especially in patients with severe periodontal diseases, in such condition extraction is being only option [1].
Intentional replantation is the deliberate removal of a tooth and its insertion into the socket immediately after proper closing the apical foramen [2]. It includes atraumatic extraction of the disturbing tooth, root-end resection/ filling, and repositioning of the extracted tooth [3]. Some authors support that, intentional replantation is seen as a last resort to save a lost tooth for other reasons [3,4]. Intentional replantation is an alternative for the treatment of advanced periodontal destruction of the anterior teeth. Grossman recommends deliberate relocation of the teeth as an alternative to extraction and placeholder replacement.5Intentional replantation is contraindicated in teeth with advanced periodontal disease and/or with large caries [5-7]. Although most of the authors support that periodontal involvement as a contraindication for replantation, some studies showed that have been successful treatment of teeth with periodontal problems [1,8]. Baykara and Eratalay [8] showed in their study, succesful survival of intentional replantation for periodontally involved teeth, they reported that there was a significant decrease in pocket depth, new bone formation and ankylosis after 8 years of follow-up [8]. Demiralp, et al. [1] intentional replanted periodontally desperate fifteen teeth, and reported that deliberate replantation could be an alternative approach to extraction for 6 months after follow-up, where advanced periodontal destruction was present and no other treatment could be considered.
Intentional replantations have been practiced in dentistry for years [2]. The intentional replantation procedure is a relatively fast and simple procedure that only gives the patient minimal discomfort after surgery [9], reducing clinical study time and has fewer possible complications and less cost compared to non-surgical endodontic treatment or dental implants [10]. The main advantage of this technique is that tooth surfaces, including inaccessible areas, can be fully visualized and used without damaging adjacent periodontal tissues and contributes to the reconstruction of healthy periradicular tissues [5,11]. Indications for intentional replantation are limited; however, in an attempt to preserve natural dentistry, it is truly a treatment option if more traditional forms of treatment fail or are impossible.2 Low cost and takes less time are advantages of this procedure. However, there is always a risk of root fracture and root resorption may occur over a period of time [12].
The aim of this case series was to demonstrate the clinical and radiographic two year results of intentional replantation of periodontally involved teeth.
In this case series, 3 patients who intentional reimplantation using the same technique are presented. Each patient received a description of the treatment procedure and signed an informed consent. All possible treatment options were explained to the patients. The risks and benefits of each option were explained in detail.
Surgical procedure
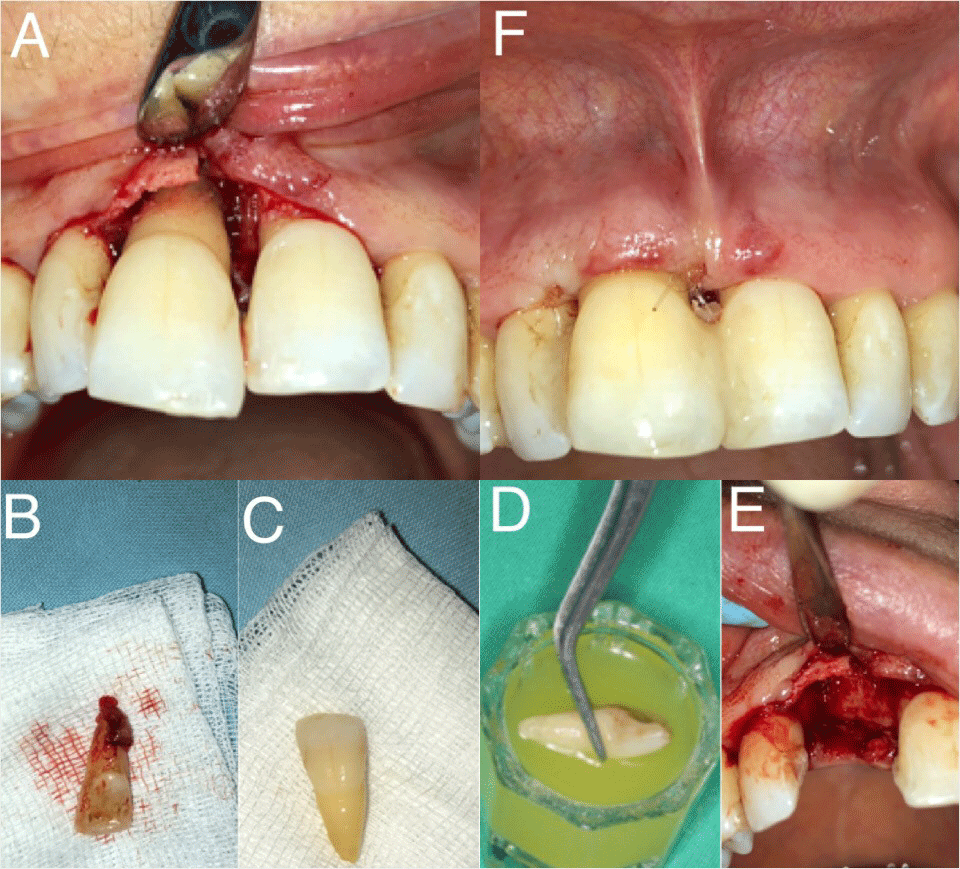
All surgical protocols were performed with the same procedure. Endodontic treatment was applied after phase-1 periodontal therapy and before the surgical procedure (Figures 1B,2B,3B). Atraumatic tooth extraction was performed by removing the flap under local anesthesia (Figure 4A). Granulation tissues in the extraction sockets were removed by gentle curettage and the sockets were rinsed with sterile saline (Figure 4B,4F). All irritants and necrotic cementum were removed from the root surfaces with periodontal curettes (Hue Friedy, Chicago ILUSA) carefully (Figure 4C).
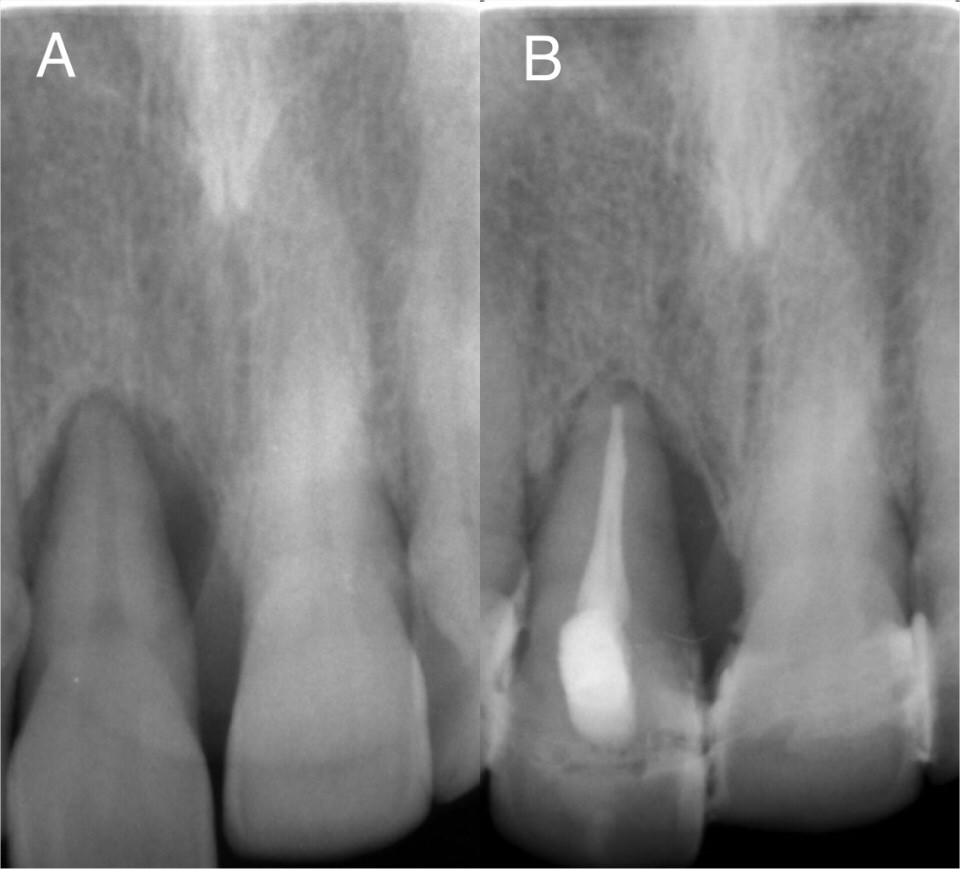
Figure 1A,B: (A) Preoperative radiograph. (B) Postoperative second year radiograph.
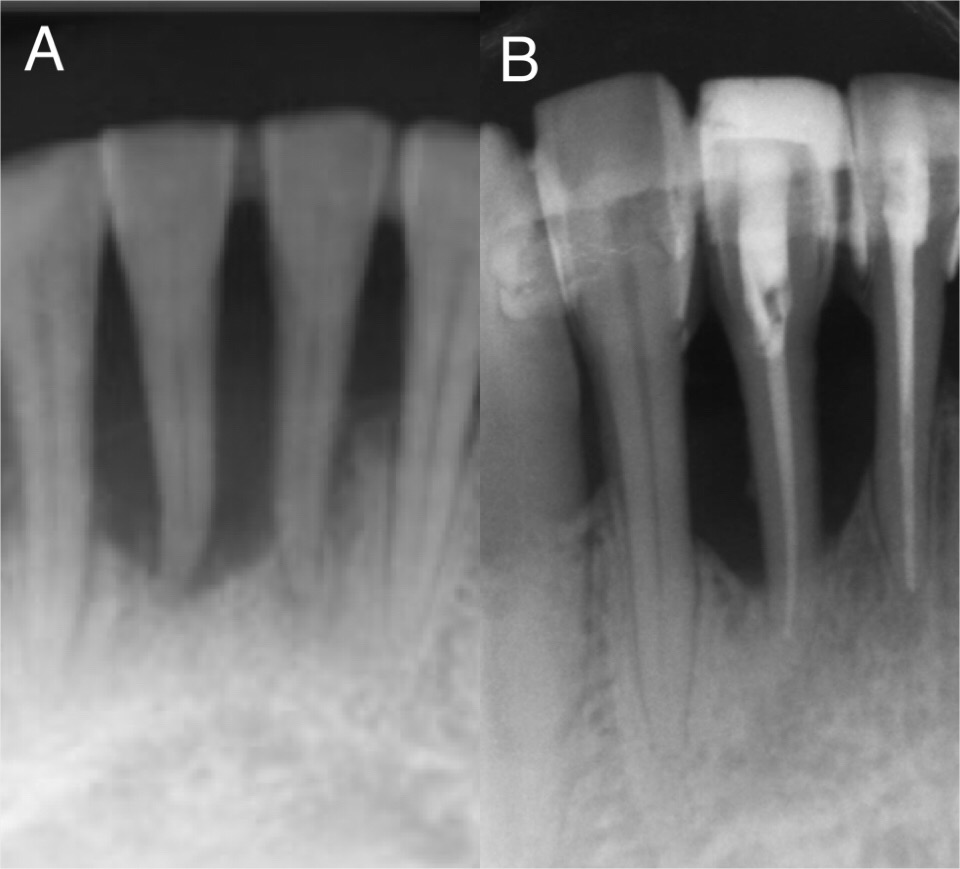
Figure 2A,B: (A) Preoperative radiograph. (B) Postoperative second year radiograph.
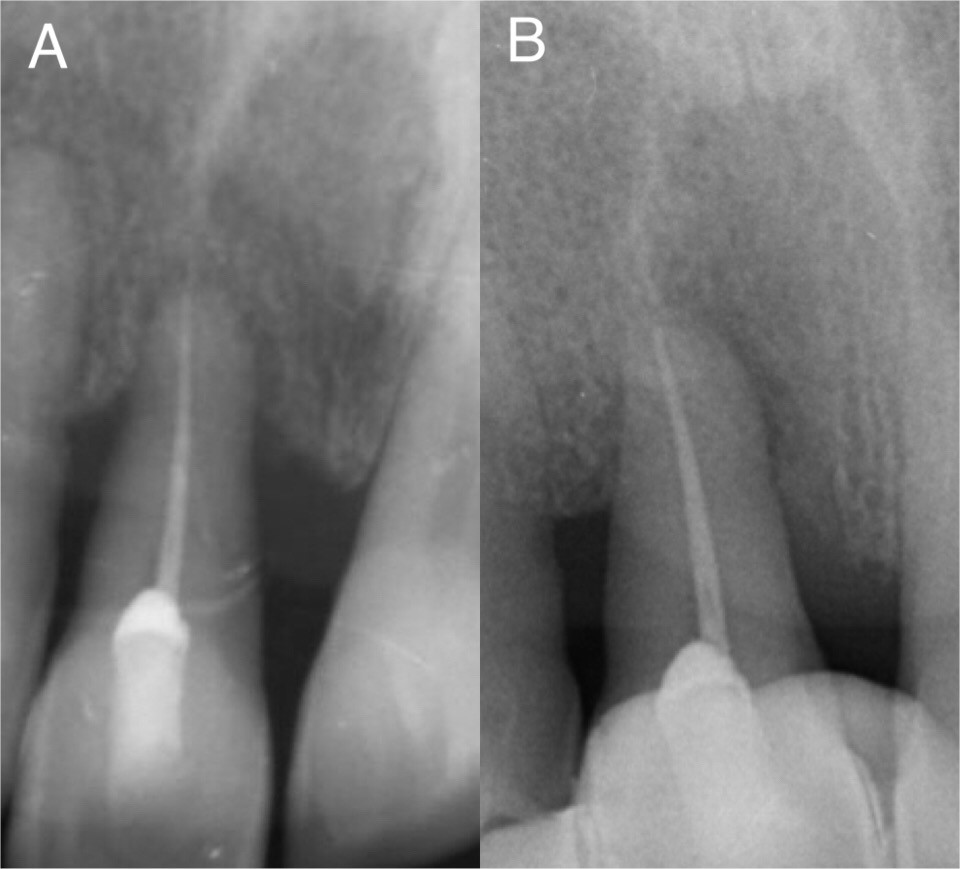
Figure 3A,B: (A)Preoperative radiograph. (B) Postoperative second year radiograph.
Figure 4A-F: Initial image. (B) Extracted tooth. (C) Cleaning of root surface. (D) Root surfacebiomodification with tetracycline. (E) Socket area (F) Splinted teeth.
After root surface correction, root bio modification was achieved by applying tetracycline HCL (100 mg/ml) to the root surface of the teeth for 5 minutes (Figure 4D).
Then, it was washed with saline for 1 minute. Care was taken not to exceed 15 minutes between extraction of the tooth and its placement in the socket. Tooth was then placed into the socket in an adequate position contacting their roots directly to the alveolar bone. The incisal edge was reshaped to prevent any occlusal trauma to occur on the tooth. To stabilize the replanted tooth, it is fixed to the side teeth from the mesial and distal contact points by composite filling material (Figure 4F).
All patients approved to have their teeth splinted during 6 months. Occlusal interferences in all centric, protrusive and lateral movements were eliminated.
Case 1
A systemically healthy, non-smoking 49-year-old female patient was admitted to clinic with complaints of mobility, pain and bleeding in the maxillary central tooth. After the clinical examination, deep periodontal pocket (≥6) [13] class III mobility 14, pathological migration and rotation were detected in the patient’s tooth # 11. Serious vertical bone loss was observed after radiological evaluations (Figure 1A).
Oral hygiene motivation was given and scaling and root planning were done as the initial periodontal therapy. At the 4th week after the initial therapy, a considerable improvement in oral hygiene and gingival health and slight reduction in periodontal pocket depths were observed during the clinical examination. Phase I treatment was completed and intentional root canal treatment was performed. The replantation procedure was planned after the completion of the root canal treatment.
Case 2
A 48-year-old woman presented to the Periodontology clinic with complaints of bleeding and excessive mobility in her lower anterior teeth (Figure 2A). There was no history of trauma and systemic disease. Pathological migration and Grade III mobility were detected in tooth 41 during intraoral and clinical examination. In periodontal probing, the pocket depth of #41 was found 8mm. Radiographic examination revealed moderate to severe bone loss in relation to #41. The female patient, who did not have any systemic disease, refused to make implants for economic reasons, demanded to protect her natural tooth and refused tooth extraction. Considering the clinical situation, intentional replantation of tooth #41 was planned after the patient was informed about the treatment and the consent form was signed. Oral hygiene motivation was given, scaling and root cleaning were done as the initial periodontal therapy. At the 4th week after the initial therapy, a considerable improvement in oral hygiene and gingival health and slight reduction in periodontal pocket depths were observed during the clinical examination. Phase I treatment was completed and intentional root canal treatment #41 was performed. Patient #41 had a deep periodontal pocket that did not respond to Phase 1 therapy, especially in the mesial. The replantation procedure was planned after the completion of the root canal treatment.
Case 3
A 63-year-old female patient was admitted to clinic with a mobility complaint in tooth #11 (Figure 3A). There was no history of trauma and systemic disease. Phase 1 periodontal treatment was applied to the patient and oral hygiene training was given. In tooth number 11, type 3 mobility was determined according to Miller classification [14]. Pocket depths of 8 mm and 10 mm were determined on the mesial and distal surfaces of the tooth, respectively. Endodontic treatment was applied to the tooth to be replanted.
Postoperative care
The patients were prescribed 100 mg of doxycycline once a day for a week and 0,2% Chlorhexidine Digluconate mouthwash twice a day. During this process, the patient were recommended to use routine oral hygiene care and an interdental toothbrush. The patients were called for control one week later. The patient was given postoperative instructions to maintain proper oral hygiene, and the patient’s oral hygiene checks were made monthly after the operation. Periodontal splints remained in the mouth for 6 months. At the end of the 6th month, clinical measurements and radiography were repeated. Periodontal pockets were clinically eliminated after 2 years of follow-up and bone gain forcase 1: 1,32 mm, for case 2: 1,37 mm for case 3: 1mm were recorded after radiological evaluations.
Patients were satisfying the replantation procedures without any complication and no postoperative discomfort were observed. Clinically, the gingiva around the involved teeth were firm and pink, and there were no bleeding during probing in all patients at the time of examination. Radiographs taken 6 months, first and second years after replantation revealed no root resorption or ankylosis were observed. Some gain in supporting bone tissue around the teeth was determined.
This case series describes the clinical and radiological consequences of the intentional replantation of teeth, which are seen as hopeless due to severe periodontal destruction. In intentionally replanted teeth, the most common causes of failure are external inflammatory resorption or replacement resorption and ankylosis caused by PDL damage and further necrosis of the PDL and cementum [9,15,16]. These complications are related to the degree of PDL damage [15,17,18]. Although no universally accepted protocol has been given for intentional replantation, various techniques and methods have been suggested by different authors [19,20].
Demiralp, et al. replanted the desperate teeth periodontally and achieved positive results at the 6th month [1]. Yaprak, et al. intentional replantation of two central teeth that were mobile due to advanced periodontal disease followed after 4 years [21]. In current cases, a similar treatment plan have been made and followed two years [22]. At the end of all procedures, patients are satisfied both aesthetically and functionally [22].
Intentional replantation may be an alternative treatment for hopeless teeth that are periodontally involved. Replanted teeth can be considered as a promising technique for keeping periodontally desperate teeth by providing healthy gums, a significant reduction in pocket depth and new bone formation that will be considered successful.
- Demiralp B, Nohutçu RM, Tepe DI, Eratalay K. Intentional replantation for periodontally involved hopeless teeth. Dent Traumatol. 2003; 19: 45-51. PubMed: https://pubmed.ncbi.nlm.nih.gov/12656855/
- Messkoub M. Intentional replantation: a successful alternative for hopeless teeth. Oral Surg Oral Med Oral Pathol. 1991; 71: 743-747.
- Bender I, Rossman LE. Intentional replantation of endodontically treated teeth. Oral Surg Oral Med Oral Pathol. 1993; 76: 623-630. PubMed: https://pubmed.ncbi.nlm.nih.gov/8247504/
- Raghoebar GM, Vissink A. Results of intentional replantation of molars. Journal of oral and maxillofacial surgery. 1999; 57: 240-244.
- Grossman LI. Intentional replantation of teeth. J Am Dent Assoc. 1966; 72: 1111-1118.
- Deeb E, Prietto PP, Mckenna RC. Reimplantation of luxated teeth in humans. J South Calif State Dent Assoc. 1965; 28: 194-206. PubMed: https://pubmed.ncbi.nlm.nih.gov/14278258/
- Healey HJ. Replantation: a brief review and a report of a case sequel. Oral Surg Oral Med Oral Pathol Oral Radiol. 1953; 6: 775-779.
- Baykara M, Eratalay K. Replantation in cases with advanced periodontal destruction. J Hacettepe Fac Dent. 1995; 19:124-128.
- Kingsbury BC, Wiesenbaugh JM. Intentional replantation of mandibular premolars and molars. J Am Dent Assoc. 1971; 83: 1053-1057. PubMed: https://pubmed.ncbi.nlm.nih.gov/5286134/
- Torabinejad M, Dinsbach NA, Turman M, Handysides R, Bahjri K, et al. Survival of intentionally replanted teeth and implant-supported single crowns: a systematic review. J Endod 2015; 41: 992-998. PubMed: https://pubmed.ncbi.nlm.nih.gov/25742795/
- Sherman P. Intentional replantation of teeth in dogs and monkeys. J Dent Res 1968; 47: 1066-1071. PubMed: https://pubmed.ncbi.nlm.nih.gov/4973663/
- Kumar A, Singh P. Intentional Replantation of Teeth: A Report of Two Cases.
- Carranza F, Camargo P. The periodontal pocket. Carranza’s clinical periodontology. 2012; 9: 349.
- Newman MG, Takei H, Klokkevold PR, Carranza FA. Carranza's clinical periodontology: Elsevier health sciences; 2011.
- Lu DP. Intentional replantation of periodontally involved and endodontically mistreated tooth. Oral Surg Oral Med Oral Pathol. 1986; 61: 508-513. PubMed: https://pubmed.ncbi.nlm.nih.gov/3459127/
- Emmertsen E. Replantation of extracted molars: preliminary report. Oral Surg Oral Med Oral Pathol. 1956; 9: 115-122.
- Weinberger BW. An introduction to the history of dentistry: With medical & dental chronology & bibliographic data: CV Mosby Company; 1948.
- Dryden JA, Arens DE. Intentional replantation. A viable alternative for selected cases. Dent Clin North Am. 1994; 38: 325-353. PubMed: https://pubmed.ncbi.nlm.nih.gov/8206180/
- Guy S, Goerig A. Intentional replantation: technique and rationale. Quintessence International, Dental Digest. 1984; 15: 595.
- Fegan S, Steiman H. Intentional replantation. J Michigan Dent Associa. 1991; 73: 22.
- Yaprak E, Hakkı S, Akman S, Belli S. Aesthetical and functional management of periodontally involved hopeless anterior teeth with multidisciplinary approach: 4 years follow-up. Dis Hekimligi Fakültesi dergisi. J Dent Faculty Ankara Univers. 19: 176-181.
- Nagappa G, Aspalli S, Devanoorkar A, Shetty S, Parab P. Intentional replantation of periodontally compromised hopeless tooth. J Indian Soc Periodontol. 2013; 17: 665-669. PubMed: https://pubmed.ncbi.nlm.nih.gov/24174765/