More Information
Submitted: December 31, 2020 | Approved: February 08, 2021 | Published: February 09, 2021
How to cite this article: Agarwal K, Lakshminarayana B. Cholecysto-colonic fistula after xanthogranulomatous cholecystitis: Surgeon’s nightmare. Arch Surg Clin Res. 2021; 5: 004-006.
DOI: 10.29328/journal.ascr.1001057
ORCiD: orcid.org/0000-0002-0762-0427
Copyright License: © Agarwal K, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Cholecysto-colonic fistula; Cholecystoenteric fistula; Xanthogranulomatous cholecystitis
Cholecysto-colonic fistula after xanthogranulomatous cholecystitis: Surgeon’s nightmare
Karan Agarwal1 and Badareesh Lakshminarayana2*
1Post Graduate, Department of Surgery, Kasturba Medical College, Manipal, India
2Associate Professor & Unit Head, Department of Surgery, Kasturba Medical College, Manipal, India
*Address for Correspondence: Badareesh L, Associate Professor & Unit Head, Department of Surgery, Kasturba Medical College, Manipal, India, Tel: +91-9844774035; Email: [email protected]; [email protected]
Xanthogranulomatous cholecystitis is a rare benign inflammatory disease of gallbladder that may be misdiagnosed as carcinoma of the gallbladder intraoperative or in pre-operative imaging. Intramural accumulation of lipid-laden macrophages and acute and chronic inflammatory cells is the hallmark of the disease. The xanthogranulomatous inflammation can be very severe and can spill over to the neighboring structures like liver, bowel and stomach resulting in dense adhesions, abscess formation, perforation, and fistulous communication with adjacent bowel [1-3]. Cholecysto-colic fistula is a rare and late complication of gallstones roughly found 1 in every 1,000 cholecystectomies.
Clinical features
The clinical features are variable and non-specific. Patients with cholecysto-colonic fistula often present with symptoms of acute cholecystitis and preoperative diagnostic tools often fail to show the fistula. Hence most cases it is an on table diagnosis.
Management
Treatment involves closing the fistula and performing an open or laparoscopic cholecystectomy.
40 year old male patient with nil premorbid illness came with complains of pain in upper abdomen since 20 days. No history of fever, jaundice or bowel/bladder disturbance. Clinical examination was unremarkable. Routine blood investigations including total leucocyte count, bilirubin levels were with in normal limits. Ultrasound abdomen and pelvis showed features suggestive of perforated gall bladder. Patient underwent CECT abdomen and pelvis (Figure 1a-c) which showed perforated emphysematous cholecystitis with cholelithiasis.
Figure 1a-c: CECT abdomen and pelvis which showed distended Gall bladder with multiple calculi in the neck of gall bladder. Fat stranding and wall thickening of gall bladder is noted. Multiple air foci are noted within the lumen and along the wall of the gall bladder. Focal defect noted along the hepatic surface of neck of gall bladder with adjacent collection measuring 5.6 x 6.3 x 3.5 cm (AP x CC x TR) abutting the inferior surface of liver superolaterally, anterior pararenal space posteriorly, second part of duodenum medially, abutting and displacing hepatic flexure of colon inferiorly.
Patient was managed conservatively with intravenous antibiotics. Patient had uneventful recovery from this attack of acute cholecystitis and was called after 6 weeks for elective laparoscopic cholecystectomy.
Patient was admitted after 6 weeks for elective laparoscopic cholecystectomy. Patients liver function test and total leucocyte count preoperatively were within normal limits. Repeat ultrasound abdomen and pelvis showed multiple gall stones with wall of gall bladder not clearly appreciated.
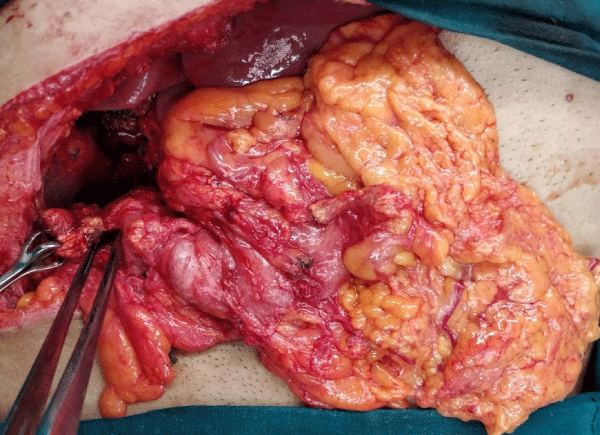
Patient was taken up for elective laparoscopic cholecystectomy. Laparoscopic cholecystectomy was converted to open procedure in view of dense adhesions between the gall bladder transverse colon and duodenum. Intraoperative shrunken and fibrotic gall bladder with multiple large calculi (Figure 2a) seen with cholecyto-transverse colon fistula (Figure 2b).
Figure 2a: Shrunken and fibrotic gall bladder with multiple large calculi.
Figure 2b: Cholecysto transverse colon fistula.
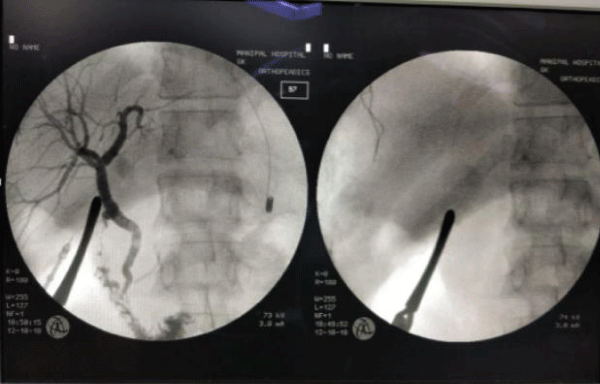
Common bile duct identification was difficult hence on table cholangiogram (Figure 2c) was done to look for any leak and check for patency of common bile. Patient underwent Subtotal cholecystectomy and primary repair of Transverse colon.
Figure 2c: On table cholangiogram – No leaks present. Filling defects in distal common bile duct.
Patient underwent Magnetic resonance cholangiopancreatography in the post-operative period, in view of filling defects in distal CBD on cholangiogram, which showed Common bile duct, common hepatic ducts and intrahepatic biliary duct radicals normal in caliber. No evidence of choledocolithiasis was there.
Post-operative recovery was uneventful. Microscopy of gall bladder and fistula tract send for histopathological examination showed extensive ulceration with few residual columnar epithelial cells surrounded by Lymphocytes, Eosinophils, sheets of foamy Histocytes and Histocytic giant cells. Final histopathology reports showed acute Xanthogranulomatous cholecystitis with rupture and fistula formation.
Biliary-enteric fistulae have been found in 0.9% of patients undergoing biliary tract surgery. The most common site is cholecystoduodenal (70%), followed by cholecystocolic (10% - 20%), and the least common is cholecystogastric fistula [5]. Spontaneous enterobiliary fistula is a complication typically associated with gallstones (90% cases) [6]. They have also been reported with abdominal trauma, Crohn’s disease, and malignancies of the biliary tract, bowel, and head of pancreas [7,8].
The exact etiology of cholecysto-colonic fistula secondary to gallstone disease is unclear. Glenn, et al. [9] proposed that acute inflammation of the gallbladder with obstruction of the cystic duct allows adhesion of the gallbladder to the contiguous organs. Recurrent acute cholecystitis promotes ulceration and ischemia of the wall of the gallbladder and the adjacent organs, resulting in further erosion and ultimately fistulation.
The most common presenting symptoms of non-obstructing biliary-enteric fistulas are abdominal pain, nausea, and diarrhea. These can be explained by the fact that cholecysto-colonic fistula alters enterohepatic circulation, leading to a malabsorption syndrome [8]. A cholecystocolonic fistula can cause a large-bowel obstruction with stone impaction at rectosigmoid diverticula [8].
Preoperative studies may include ultrasound, CT scan, MR, ERCP, and barium enema, but a proper diagnosis is often achieved intraoperative [10]. Pneumobilia may give a suspicion of cholecysto-colonic fistula [8] especially if the gallbladder is atrophic and anatomically adjacent to another organ on computed tomography or ultrasound. However, Yamashita, et al. [11] reported that ERCP was the most accurate diagnostic modality of cholecysto-colonic fistula. Wang, et al. [12] were able to illustrate cholecysto-colonic fistula using ultrasound, ERCP, and magnetic resonance imaging techniques in 50% of cases.
Standard treatment of cholecysto-colonic fistula is open cholecystectomy and closure of fistula. As a result of increasing surgical expertise, laparoscopic surgery can now be used in fistula treatment. Results have shown no significant difference in intraoperative and postoperative complications with the proper surgical technique [13-15].
Laparoscopic cholecystectomy following an episode of cholecystitis especially after xanthgranulomatous inflammation requires extreme care to identify and treat fistulas to avoid life-threatening events thereafter.
- Yucel O, Uzun MA, Tilki M, Alkan S, Kilicoglu ZG, et al. Xanthogranulomatous Cholecystitis: Analysis of 108 Patients. Indian J Surg. 2017; 79: 510-514. PubMed: https://pubmed.ncbi.nlm.nih.gov/29217901/
- Christensen AH. Benign tumors and pseudotumors of the gallbladder. Report of 180 cases. Arch Pathol. 1970; 90: 423-432. PubMed: https://pubmed.ncbi.nlm.nih.gov/4319984/
- Goodman ZD, Ishak KG. Xanthogranulomatous cholecystitis. Am J Surg Pathol. 1981; 5: 653-659. PubMed: https://pubmed.ncbi.nlm.nih.gov/7337158/
- Glenn F, Reed C, Grafe WR. Biliary enteric fistula. Surg Gynecol Obstet. 1981; 153: 527-531. PubMed: https://pubmed.ncbi.nlm.nih.gov/7280941/
- Rigler LG, Borman CN, Noble JF. Gallstone obstruction: pathogenesis and roentgen manifestations. J Am Med Associat. 1941; 117: 1753-1759.
- Costi R, Randone B, Violi V, Scatton O, Sarli L, et al. Cholecystocolonic fistula: facts and myths. A review of the 231 published cases. J Hepatobiliary Pancreat Surg. 2009; 16: 8-18. PubMed: https://pubmed.ncbi.nlm.nih.gov/19089311/
- Chandar VP, Hookman P. Choledochocolonic Fistula Through a Cystic Duct Remnant. Am J Gastroenterol. 1980; 74: 179-181. PubMed: https://pubmed.ncbi.nlm.nih.gov/7446519/
- LeBlanc KA, Barr LH, Rush BM. Spontaneous biliary enteric fistulas. South Med J. 1983; 76: 1249-1252. PubMed: https://pubmed.ncbi.nlm.nih.gov/6623136/
- Glenn F, Reed C, Grafe WR. Biliary enteric fistula. Surg Gynecol Obstet. 1981; 153: 527-531. https://pubmed.ncbi.nlm.nih.gov/7280941/
- Angrisani L, Corcione F, Tartaglia A, Tricarico A, Rendano F, et al. Cholecystoenteric fistula (CF) is not a contraindication for laparoscopic surgery. Surg Endoscopy. 2001; 15: 1038-1041. PubMed: https://pubmed.ncbi.nlm.nih.gov/11443421/
- Yamashita H, Chijiiwa K, Ogawa Y, Kuroki S, Tanaka M. The internal biliary fistula–reappraisal of incidence, type, diagnosis and management of 33 consecutive cases. HPB Surgery. 1997; 10: 143-147. PubMed: https://pubmed.ncbi.nlm.nih.gov/9174858/
- Wang WK, Yeh CN, Jan YY. Successful laparoscopic management for cholecystoenteric fistula. World J Gastroenterol. 2006; 12: 772-775. PubMed: https://pubmed.ncbi.nlm.nih.gov/16521193/
- Conde LM, Tavares PM, Quintes JL, Chermont RQ, Alvarez Perez MC. Laparoscopic management of cholecystocolic fistula. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo). 2014; 27: 285-287. PubMed: https://pubmed.ncbi.nlm.nih.gov/25626940/
- Ha GW, Lee MR, Kim JH. Cholecystocolic fistula caused by gallbladder carcinoma: Preoperatively misdiagnosed as hepatic colon carcinoma. World J Gastroenterol. 2015; 21: 4765-4769. PubMed: https://pubmed.ncbi.nlm.nih.gov/25914489/
- Gora N, Singh A, Jain S, Parihar US, Bhutra S. Spontaneous cholecystocolic fistula: case report. J Clin Diagn Res. 2014; 8: 164-165. PubMed: https://pubmed.ncbi.nlm.nih.gov/24783121/