More Information
Submitted: October 03, 2021 | Approved: October 14, 2021 | Published: October 15, 2021
How to cite this article: Karahan F, Acar N, Avcı A, Dilek ON. Coexistence of common gallstones and sinusoidal obstruction syndrome: Case report and review of the literature. Arch Surg Clin Res. 2021; 5: 020-022.
DOI: 10.29328/journal.ascr.1001060
Karahan F: orcid.org/0000-0003-0384-8181
Acar N: orcid.org/0000-0003-0720-3794
Avcı A: orcid.org/0000-0002-5522-0022
Dilek ON: orcid.org/0000-0002-6313-3818
Copyright License: © Karahan F, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Sinusoidal obstruction syndrome; Diagnosis; Gallstones; Treatment; Veno-occlusive disease
Coexistence of common gallstones and sinusoidal obstruction syndrome: Case report and review of the literature
Furkan Karahan1*, Nihan Acar1, Arzu Avcı2 and Osman Nuri Dilek1
1IKCU Ataturk Training and Research Hospital, Departments of General Surgery, İzmir, Turkey
2IKCU Ataturk Training and Research Hospital, Departments of Medical Pathology, Turkey
*Address for Correspondence: Dr. Furkan Karahan, Departments of General Surgery, IKCU Ataturk Training and Research Hospital, Izmir, Turkey, Email: [email protected]
Purpose: The sinusoidal obstruction syndrome (SOS) of the liver is an obliterative vasculitis that involves the terminal branches of the hepatic venules and sinusoids. When it is not treated, it will be a serious risk of mortality. Here, we aim to present our patient who has been associated with recurrent cholangitis attacks due to cholelithiasis and choledocholithiasis and is associated with sinusoidal obstruction syndrome with the literature.
Description of the case: A 30 years old male patient had complaints of abdominal pain and nausea for a long time. The patient had a history of choledocholithiasis and cholangitis attacks. Although ERCP was performed and a stent was placed in the biliary tract, his jaundice did not disappear. Liver function tests were high. Tumor markers were negative.
Methods: We could not make a definitive diagnosis with imaging methods and biopsy and we planned surgery. We performed segmental liver resection and biliary diversion in the surgery. Histopathological examination of the resected liver tissue was compatible with SOS.
Conclusion: Many studies have been done on the etiology of SOS and different causes have been revealed. Accompanied with clinical findings, a definitive diagnosis is made with the exclusion of the presumptions considered. Surgery can be performed for both diagnostic and therapeutic purposes. If patients with elevated liver function tests and bilirubin have long-term abdominal pain, SOS should be bear in mind.
Sinusoidal obstruction syndrome (SOS), also known as hepatic veno-occlusive disease (VOD), is a clinical finding characterized by hepatomegaly, jaundice and intra-abdominal acid associated with abdominal pain attacks [1]. While it is most seen in the Western countries after hematopoietic stem cell transplantation (HSCT), the uptake of plants containing pyrolysidine alkaloids in the far east is the main etiologic factor. SOS cases have been reported, especially in those consuming tusanqi plants containing pyrolysidine alkaloids in China [2]. Regardless of the cause, the main pathology in these is the toxic damage of sinusoidal endothelial cells. Recent studies have found an increase in CD34 expression in the sinusoidal cells of these patients, and it has been shown that this correlates with the severity of SOS [3].
Initially painful hepatomegaly, jaundice, weight gain and acid are common symptoms. Serum transaminase levels increase but are not specific. Especially in severe SOS cases secondary to HSCT, multiorgan disease (MOD) and high mortality (80%) can be seen. This rate is over 90% in cases with high bilirubin value and weight gain [4]. The final diagnosis is made by exclusion of other findings and liver biopsy.
Here, we aimed to present our patient, who came with recurrent cholangitis attacks due to cholelithiasis and choledocholithiasis and was associated with sinusoidal obstruction syndrome in the light of literature data.
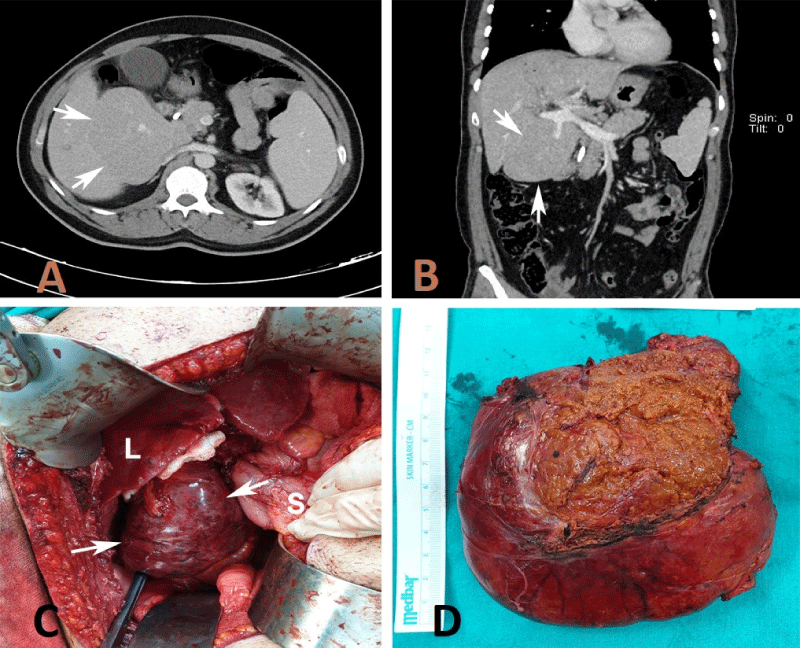
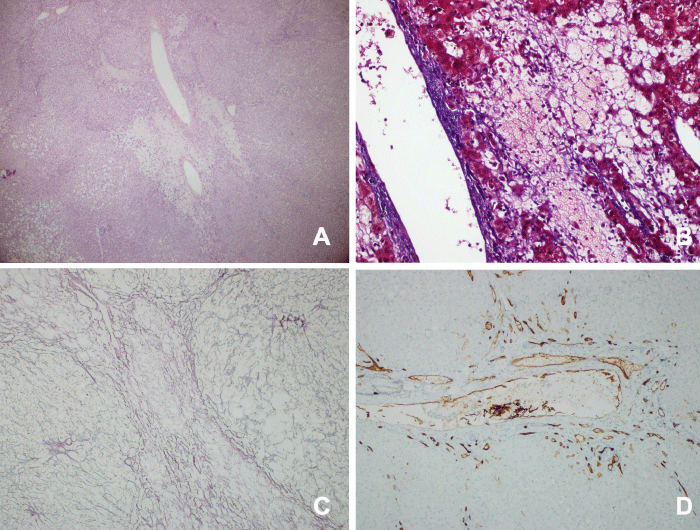
A 30 years old male patient presented with a complaint of abdominal pain and nausea for about one year. There were previous attacks of cholecystitis and cholangitis. In his history, it was learned that many endoscopic retrograde cholangiopancreatography (ERCP) procedures have been performed in the last 4 years due to cholelithiasis, choledocholithiasis and hepatolithiasis. In terms of biliary drainage, external and internal catheters were implanted in the biliary tract many times (Figure 1A-B). There were no known additional diseases and previous abdominal surgery. Physical examination revealed jaundice in the sclera and tenderness in the epigastrium. In laboratory examination, AST:80 U/L (5-34 U/L), ALT:192 U/L (0-55 U/L), ALP:249 U/L (40-150 U/L), GGT:512 U/L (12-64 U/L), total bilirubin: 1.8 mg/dL, tumor and hepatitis markers were negative. In computed tomography (CT) and magnetic resonance imaging (MRI), liver parenchyma was found to be heterogeneous in different densities, although no clear mass lesion was observed (Figure 1A-B). He had hepatosplenomegaly. The operation was planned for the patient who had intermittent jaundice and abdominal pain attacks althoughit was benign as a result of tru-cut biopsy taken from the liver. On the back of the liver, a hyperplastic tissue with a hemangioma appearance of 10x8 cm in size ranging from segment 6 to segment 7 and vena cava was resected (Figure 1C-D). When choledoctomy was performed, the choledochal wall was found to be thick and edematous. Millimeter stones and debris were cleared. The operation was terminated by performing cholecystectomy and choledocoduodenostomy. The patient, who had no problem in subsequent follow-up, was discharged on the 7th postoperative day. In the histopathological examination of the specimen, it was observed that the liver resection material contained nodular structure and hemorrhagic areas. The central vein was dilatation and pericentral areas were edema. CD34 expression was detected to be increased (Figure 2A-B-C-D). With these findings, it was evaluated as venoocclusive disease of the liver. In the 9-month follow-up of the patient, no recurrence or complications were detected in abdominal discomfort and liver enzymes (AST, ALT), except elevation.
Figure 1: A-B: In the abdominal CT axial and coronal sections, there is a mass image (Arrows) showing different enhancement and heterogeneity extending from segment 6-7 to the liver hilum (Top row). C-D: The resected specimen (Left) and appearance of the exophytic mass just under the liver in the operation (Bottom row, Right).
Figure 2: A: Congestion, extravased erythrocytes and edema, H&E, x10. B: Collagen accumulation in pericentral area (-), edema (+), Massontrikrom, x20. C: Collapsed pericentral reticular roof, reticulum, x10. D: Endothelial immun expression in vascular structures, CD34, x20.
Sinusoidal obstruction syndrome was first seen in 1954 in those who consumed herbal teas containing pyrolysidine and was also defined as VOD due to the detection of lesions in the liver terminal venules microscopically [1]. However, in subsequent studies, it was understood that radicals damaged the first hepatic sinusoids and that fibrosis caused obstruction in central veins and was called SOS. The reported incidence is in a wide range. While the incidence of SOS is 9.1% in patients receiving chemotherapy due to acute myeloid leukemia (AML), it is 39% in patients receiving chemotherapy due to liver metastasis of colorectal cancer. Its incidence after hematopoietic stem cell transplantation (HSCT) is between 5 and 60%. In the formation of this wide range; The etiology of SOS, the presence of various risk factors and the criteria used in diagnosis are effective [3,5,6].
The diagnosis and etiology change of SOS can be made by excluding possible causes according to clinical findings [1,3]. Although it was rarely seen before, recently increasing hematopoietic transplantations, adjuvant / neoadjuvant therapies and consumption of herbal teas of unknown origin have increased the incidence. After all cases of SOS developing due to long-term use of azathiopurine after organ transplantation have been reported [6]. However, there is no literature data about its association with bile duct stones. There are studies on the increase in wall thickness in the gallbladder as a predictor factor for SOS [7]. In addition, the use of Ursodeoxycholic acid (UDCA), which reduces gallstone formation, in SOS treatment may show its relevance to gallstones. In our detailed research and inquiry, no etiological factor other than bile duct stones was found in our patient.
Imaging methods and scoring systems can help diagnose the disease. Today, non-invasive methods such as US, CT and MRI have been used more in diagnosis and follow-up. Also, supersonic wave imaging (SSI) and bipolar CT (DECT) showing perfusion change, which assesses liver stiffness, are promising in the diagnosis of SOS. Animal experiments conducted by Shin et al. have demonstrated that SSI and DECT can help in the early diagnosis of SOS without structural changes in the liver [2]. But, histopathological examination is still the gold standard method in the diagnosis of SOS [8]. The difficulty of application of the procedure and the risk of bleeding and infection afterward are the negative aspects of liver biopsy. As a result of the histopathological evaluation, we reached a definitive diagnosis in this patient, whom we could not diagnose using imaging methods.
There is no standard and effective approach to treatment. The goal is to eliminate the cause of SOS and alleviate the symptoms. Defibrotide is a new agent that acts on adenosine receptors. It has shown successful results in the medical treatment of SOS due to its decrease in small vessel endothelial damage and antithrombotic effect. In addition, the use of defibrotide is thought to increase survival in patients with MODS after SOS. In the study of Richardson et al. in patients who developed VOD/SOS after HSCT, it was revealed that the use of defibrotide increased the 100-day survival regardless of the severity of MODS. In the same study, it was stated that starting the drug early without severe organ dysfunctions such as ventilator and dialysis dependence will improve the results [1]. Apart from this, UDCA, a hydrophilic bile acid, is used in SOS treatment and prophylaxis with the production of proinflammatory cytokines and the fraction reducing the effect of hepatotoxic bile acids. In the study performed by Tay, et al. on the prophylactic UDCA, it was reported that it significantly reduced the incidence of SOS especially in patients undergoing HSCT [7]. In the case of severe portal hypertension, portosystemic shunts can be tried to reduce pressure. Segmented liver resection can be performed in patients with sinusoidal injury and venous fibrosis-related parenchymal damage. In our patient, non-anatomical segmental resection was performed.
In our patient’s anamnesis and background information; None of the factors mentioned in etiology such as hematopoietic stem cell transplantation, history of chemotherapy or radiotherapy to the liver, history of chemotherapy due to AML and solid organ transplantation. The intake of nutrients and herbal teas containing prolyzidine alkaloids has been specifically questioned, but no exposure has been detected. Hepatitis markers were negative. His clinic had jaundice, painful hepatomegaly, and common gallstones. No signs of weight gain, intraabdominal acid and portal hypertension were not detected. After multiple ERCPs and biliary stenting, liver and cholestasis enzymes remained high. In these conditions, it was seen that bilirubin values regressed after surgery performed for diagnosis and treatment. No literature information about common and recurrent gallstones was found in SOS etiology. The association of common bile duct stones and SOS, in this case, is significant in terms of being the first.
Although there are no reasons stated in the etiology, SOS should be kept in mind in patients with high levels of cholestasis with liver function tests, hyperbilirubinemia and abdominal pain episodes, and after performing other causes, liver biopsy should be performed. Although there is currently no standard treatment approach, we think that patients with biliary stenosis and symptomatic patients will benefit from surgery.
- Richardson PG, Smith AR, Kernan NA, Lehmann L, Soiffer RJ, et al. Pooled analysis of Day 100 survival for defibrotide-treated patients with hepatic veno-occlusive disease/sinusoidal obstruction syndrome and ventilator or dialysis dependence following haematopoietic cell transplantation. Br J Haematol. 2020; 190: 583-587. PubMed: https://pubmed.ncbi.nlm.nih.gov/32157682/
- Shin J, Yoon H, Cha YJ, Han K, Lee MJ, et al. Liver stiffness and perfusion changes for hepatic sinusoidal obstruction syndrome in rabbit model. World J Gastroenterol. 2020; 26: 706-716. PubMed: https://pubmed.ncbi.nlm.nih.gov/32116418/
- Zhang Y, Yan Y, Song B. Noninvasive imaging diagnosis of sinusoidal obstruction syndrome: a pictorial review. Insights Imaging. 2019; 10: 110. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6868080/
- McDonald GB, Sharma PANKAJ, Matthews DE, Shulman HM, Thomas ED. The clinical course of 53 patients with venocclusive disease of the liver after marrow transplantation. Transplantation. 1985; 39: 603-608. PubMed: https://pubmed.ncbi.nlm.nih.gov/3890288/
- Mohty M, Malard F, Abecassis M, Aerts E, Alaskar AS, et al. Revised diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: a new classification from the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant. 2016; 51; 906-912. PubMed: https://pubmed.ncbi.nlm.nih.gov/27183098/
- Tallman MS, McDonald GB, DeLeve LD, Baer MR, Cook MN, et al. Incidence of sinusoidal obstruction syndrome following Mylotarg (gemtuzumab ozogamicin): a prospective observational study of 482 patients in routine clinical practice. Int J Hematol. 2013; 97: 456-464. PubMed: https://pubmed.ncbi.nlm.nih.gov/23460018/
- Tay J, Tinmouth A, Fergusson D, Huebsch L, Allan DS. Systematic review of controlled clinical trials on the use of ursodeoxycholic acid for the prevention of hepatic veno-occlusive disease in hematopoietic stem cell transplantation. Biol Blood Mar Trans. 2007; 13: 206-217. PubMed: https://pubmed.ncbi.nlm.nih.gov/17241926/
- Park JE, Choi YH, Cheon JE, Kim WS, Kim IO, et al. Gallbladder wall oedema and ascites are independent predictors of progression to hepatic veno-occlusive disease for children with hematopoietic stem cell transplantation. Eur Radiol. 2018; 28: 2291-228. PubMed: https://pubmed.ncbi.nlm.nih.gov/29294155/