More Information
Submitted: March 13, 2023 | Approved: March 17, 2023 | Published: March 20, 2023
How to cite this article: Jacob S, Ahluwalia C. A case of true hermaphroditism: presenting as congenital bilateral inguinal hernia. Arch Surg Clin Res. 2023; 7: 001-003.
DOI: 10.29328/journal.ascr.1001066
Copyright License: © Jacob S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A case of true hermaphroditism: presenting as congenital bilateral inguinal hernia
Sherrin Jacob and Charanjeet Ahluwalia*
MMC and Safdarjung Hospital, New Delhi-110029, India
*Address for Correspondence: Charanjeet Ahluwalia, VMMC and Safdarjung Hospital, New Delhi-110029, India, Email: [email protected]
True hermaphroditism (TH) is a cause of intersexuality in which both ovarian and testicular tissue is present in the same individual [1]. The gonadal distribution in cases of true hermaphroditism varies from [2],
- Lateral true hermaphroditism- Ovary on one side and testis on the other
- Unilateral true hermaphroditism- Ovotestis on one side and ovary on other
- Bilateral true hermaphroditism- Ovotestis on both sides.
The exact incidence of true hermaphroditism remains unclear, however, approximately 500 cases have been reported worldwide. True hermaphroditism is the rarest variety (5%) in the spectrum of Disorder of Sexual Development (DSD) [3]. The most common chromosomal composition in true hermaphrodites is 46, XX followed by 46, XX/46, XY mosaicism [4]. Other rarely found karyotypes are 46, XY; 46, XXY, etc. The most important differential diagnosis of true hermaphroditism having clinical implications is mixed gonadal Dysgenesis (MGD) [5]. In contrast to true hermaphroditism, MGD has characterized the presence of streak gonads on one side and a mature developed gonad (commonly, testis) on the other. Early gonadectomy is indicated in patients of MGD to prevent the occurrence of malignant germ cell tumors [6]. Rare incidences of malignancies like gonadoblastoma and dysgerminoma in patients of true hermaphroditism have also been reported. Recently, a case of sex cord tumor with annular tubules (SCTAT) has been reported in a patient with true hermaphroditism [7].
This case report documents a two-year-old child of true hermaphroditism with an extremely rare presentation of bilateral inguinal hernia.
Clinical presentation
A two-year-old child raised as a female presented with bilateral inguinal swelling since birth which became prominent on crying and straining during the passage of stools. The swelling was reducible and the cough impulse was positive. External genital examination revealed only one opening in the vestibule which was the urethral opening. No clitoris, vagina, or vaginal pit was identified.
Ultrasonographic examination
On the USG of the pelvis, no uterus was identified. Homogenous solid nodules were identified in both inguinal rings. Tubes arising from these solid nodules were seen ending in the bladder neck. Based on ultrasonographic and clinical findings, a provisional diagnosis of Androgen Insensitivity Syndrome was suggested.
Operative findings
On laparoscopic bilateral inguinal hernial repair, bilateral gonads were identified as prolapsing through the open deep inguinal ring. The left gonad was 2 × 2 cm and the right gonad was 1 × 0.6 cm, both showing bluish dots on the surface probably representing the presence of follicles. However, no Mullerian structures were identified. Vas-like tubal structures were identified arising from both gonads, going medially and ending on the bladder neck. The hernia was repaired and a right gonadal biopsy was taken.
Histopathological examination
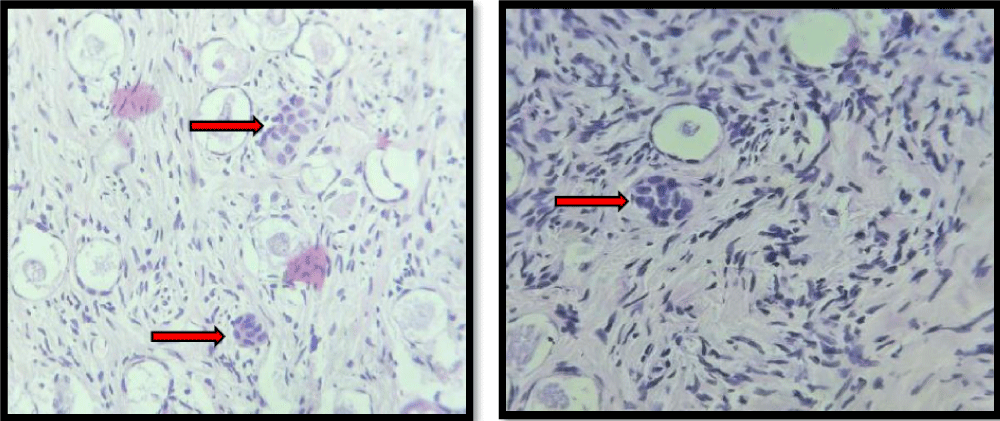
Histopathological examination from the biopsy showed the presence of ovarian stroma and primordial follicles. There were primitive seminiferous tubules intermixed in the ovarian stromal tissue. The gonadal tissue was identified as Ovotestis characteristic of True hermaphroditism (Figure 1).
Figure 1: Primitive seminiferous tubules (red arrow) intermixed with ovarian stroma and follicles.
Postoperative period
Postoperative period was uneventful. The patient was started on oral food from day 2 postoperatively. The patient was tolerating oral feed and passing urine and stools. She was afebrile, and her abdomen was soft. The patient was advised to follow up and karyotyping on discharge.
Genes responsible for gonadal differentiation include: Sex- determining the Region of chromosome Y (SRY) encoded by chromosome Yp11.2, Anti- Mullerian Hormone (AMH) gene encoded by 19p13.3, Steroidogenic Factor (SF), Dose -sensitive sex reversal congenital adrenal dysplasia (DAX) gene, and Sex determining region Y box Protein 9 (SOX 9) encoded by 17q24 [7]. Abnormal change in any of the above-known genes lead to the occurrence of true hermaphroditism. Other known environmental factors include exposure to exogenous estrogen or progesterone during pregnancy. The most common presentation of TH is abnormal external genitalia followed by haematuria, cryptorchidism, and amenorrhea [8]. True hermaphroditism in a child reared as a female presenting with a congenital bilateral inguinal hernia is an extremely rare presentation as in our case. Definitive early gender assignment is one of the main aspects to be addressed in cases of True hermaphroditism diagnosed in children. In most cases, the gender assigned is the same as the gender in which the child is reared. A simple classification was designed based on the external genitalia to assign gender to the child as follows [9]:
- Class I- Normal female genitalia
- Class II- enlarged clitoris
- Class III- partially fused labioscrotal folds
- Class IV- completely fused labioscrotal folds
- Class V- Hypoplastic scrotum and penoscrotal hypospadias
- Class VI- Normal male genitalia.
This classification recommends that all true herma-phrodites of class I to IV be raised as females and only V and VI with strong male genitalia be raised as males. This is based on the ability to satisfactorily reconstruct the genital anatomy.
Once diagnosed, these patients should be advised to follow up due to the possibility of malignant changes in the gonads. Case of a 49-year-old woman with a genotype of 46, XY had a mass in the inguinal region for 30 years. The mass in the left inguinal region was diagnosed as dysgerminoma and the mass in the right inguinal mass was diagnosed as cryptorchidism [10]. Similarly, cases of seminoma, gonadoblastoma, and Sex cord tumor with annular tubules have been reported in patients of true hermaphroditism [7,11,12]. Histopathological examination of gonads is of utmost importance in these cases for accurate diagnosis and long-term management of the patients.
To our knowledge, only one other case of a 21-year-old true hermaphrodite male with normal external genitalia presenting with an inguinal hernia has been reported [13].
Author contribution
Sherrin Jacob and Charanjeet Ahluwalia recognized the entity and proposed the writing. Sherrin Jacob wrote the paper. The paper was edited and reviewed by Charanjeet Ahluwalia.
Compliance with ethical standards
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
- Yordam N, Alikasifoglu A, Kandemir N, Caglar M, Balci S. True hermaphroditism: clinical features, genetic variants and gonadal histology. J Pediatr Endocrinol Metab. 2001 Apr;14(4):421-7. doi: 10.1515/jpem.2001.14.4.421. PMID: 11327376.
- van Niekerk WA, Retief AE. The gonads of human true hermaphrodites. Hum Genet. 1981;58(1):117-22. doi: 10.1007/BF00284158. PMID: 6895206.
- Iqbal MZ, Jam MR, Saleem M, Ahmad M. True hermaphrodite: a case report. APSP J Case Rep. 2011 May;2(2):16. Epub 2011 Jul 30. PMID: 22953283; PMCID: PMC3418019.
- Krob G, Braun A, Kuhnle U. True hermaphroditism: geographical distribution, clinical findings, chromosomes and gonadal histology. Eur J Pediatr. 1994 Jan;153(1):2-10. doi: 10.1007/BF02000779. PMID: 8313919.
- Kim KR, Kwon Y, Joung JY, Kim KS, Ayala AG, Ro JY. True hermaphroditism and mixed gonadal dysgenesis in young children: a clinicopathologic study of 10 cases. Mod Pathol. 2002 Oct;15(10):1013-9. doi: 10.1097/01.MP.0000027623.23885.0D. PMID: 12379746.
- Zäh W, Kalderon AE, Tucci JR. Mixed gonadal dysgenesis. Acta Endocrinol Suppl (Copenh). 1975;197:1-39. PMID: 1094776.
- Shi S, Tang M, Li W, Wu H, Liu Y, Luo Y, Ding H. True hermaphroditism with sex cord tumor with annular tubules (SCTAT): a rare case report and review of the literature. BMC Womens Health. 2022 Dec 27;22(1):551. doi: 10.1186/s12905-022-02137-7. PMID: 36575516; PMCID: PMC9793495.
- van Niekerk WA. True hermaphroditism: an analytic review with a report of 3 new cases. Am J Obstet Gynecol. 1976 Dec 1;126(7):890-907. PMID: 1033669.
- Luks FI, Hansbrough F, Klotz DH Jr, Kottmeier PK, Tolete-Velcek F. Early gender assignment in true hermaphroditism. J Pediatr Surg. 1988 Dec;23(12):1122-6. doi: 10.1016/s0022-3468(88)80326-9. PMID: 3236177.
- Chen CQ, Liu Z, Lu YS, Pan M, Huang H. True hermaphroditism with dysgerminoma: A case report. Medicine (Baltimore). 2020 May 29;99(22):e20472. doi: 10.1097/MD.0000000000020472. PMID: 32481455.
- Lai Y, Xie J, Tian P, Zhong L, Ni L. True hermaphroditism with seminoma: A case report. Mol Clin Oncol. 2019 Jan;10(1):97-100. doi: 10.3892/mco.2018.1760. Epub 2018 Nov 8. PMID: 30655982; PMCID: PMC6313949.
- Mondal S, Chatterjee K, Bhattacharya SK, Nath SK. Ovarian germ cell neoplasm in a true hermaphrodite. J Indian Med Assoc. 2011 Nov;109(11):832-3, 835. PMID: 22666943.
- Ceylan K, Algun E, Gunes M, Gonulalan H. True hermaphroditism presenting as an inguinal hernia. Int Braz J Urol. 2007 Jan-Feb;33(1):72-3. doi: 10.1590/s1677-55382007000100011. PMID: 17335601.