More Information
Submitted: April 20, 2023 | Approved: May 02, 2023 | Published: May 03, 2023
How to cite this article: Reveron-Thornton R, Norton J. Results of a prospective strategy for focused Minimally Invasive Parathyroidectomy (MIP). Arch Surg Clin Res. 2023; 7: 016-018.
DOI: 10.29328/journal.ascr.1001069
Copyright License: © Reveron-Thornton R, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Results of a prospective strategy for focused Minimally Invasive Parathyroidectomy (MIP)
Rosyli Reveron-Thornton and Jeffrey Norton*
257 Campus Drive, Stanford, CA 94305, USA
*Address for Correspondence: Jeffrey Norton, Department of Surgery, Division of General Surgery, Stanford University School of Medicine, 257 Campus Drive, Stanford, CA 94305, USA, Email: [email protected]
Neck exploration for primary HPT is the standard operation in which 4 parathyroid glands are identified and one abnormal parathyroid gland is removed. This is recommended for all patients with primary HPT. We hypothesized that most patients with primary HPT have a single abnormal parathyroid gland (adenoma) and parathyroid imaging studies will identify it and support a focused minimally invasive parathyroidectomy (MIP). This can be combined with ioPTH monitoring making bilateral exploration unnecessary. This paper reports a 93.4% success rate in 249 consecutive prospective patients with primary HPT over a 15-year period with a short operating time and few complications. The findings suggest that this alternate surgical MIP approach should be the procedure of choice for HPT patients.
The standard surgical strategy for primary hyperparathyroidism (HPT) is bilateral cervical exploration, abnormal gland excision, and normal gland biopsy. Currently, surgical intervention is indicated for patients with symptomatic HPT or in asymptomatic patients meeting the 2002 and 2009 NIH consensus panel guidelines [1]. Reoperative parathyroid surgery in patients who develop recurrent HPT after prior neck exploration has demonstrated that radiologic imaging studies can correctly localize most parathyroid adenomas [2]. Further, the development of intraoperative PTH (ioPTH) determinations can document whether or not a successful outcome has occurred during surgery [2]. In 2005, we hypothesized that intraoperative radioimmunoassays for parathyroid hormone (ioPTH) and localizing imaging studies (ultrasound, 99mTc sestamibi scan, and 4D/computed tomography) allow successful employment of a focused unilateral minimally invasive parathyroidectomy (MIP) that would cause minimal complications and less pain with similar success. Thus, potential benefits of MIP are smaller incisions, shorter operating time, and similar success rates. In this study, we report the results of MIP in a large prospective cohort of consecutive patients with primary HPT.
Between 2005-2020, 393 consecutive HPT patients underwent diagnostic confirmation (concomitant elevated serum calcium and PTH levels) and localizing studies (99 mTc sestamibi, ultrasound, and 4-D CT when available) prior to neck surgery. 249 (63%) patients had positive localization studies and underwent a focused, unilateral, minimally invasive parathyroidectomy (MIP) on the side of the neck defined by the preoperative localization results. A 3 cm transverse incision was focused on the medial border of the sternocleidomastoid muscle (SCM). The incision was made through the skin and platysma muscle. Subplatysmal flaps were raised both superiorly and inferiorly. The neck was explored by opening along the medial border of the SCM muscle. The thyroid lobe was elevated with a Babcock clamp and dissection was done posterior to the thyroid. Care was taken to identify and preserve the recurrent laryngeal nerve. Occasionally the inferior strap muscles were divided to facilitate the elevation of the thyroid lobe. ioPTH blood levels were measured at the beginning of the case, immediately following the removal of an abnormal parathyroid gland, and 10 minutes later. An ioPTH decrease of at least 50% from the baseline value and/or into the normal range after 10 minutes from parathyroid gland excision defined a successful outcome. Any abnormal parathyroid gland excised was confirmed by frozen pathological assessment. Abnormal parathyroid tissue on the frozen section and a 50% drop in serum PTH level after the removal of an abnormal parathyroid gland was used to define a successful result. Proportions are compared by Fisher’s exact test.
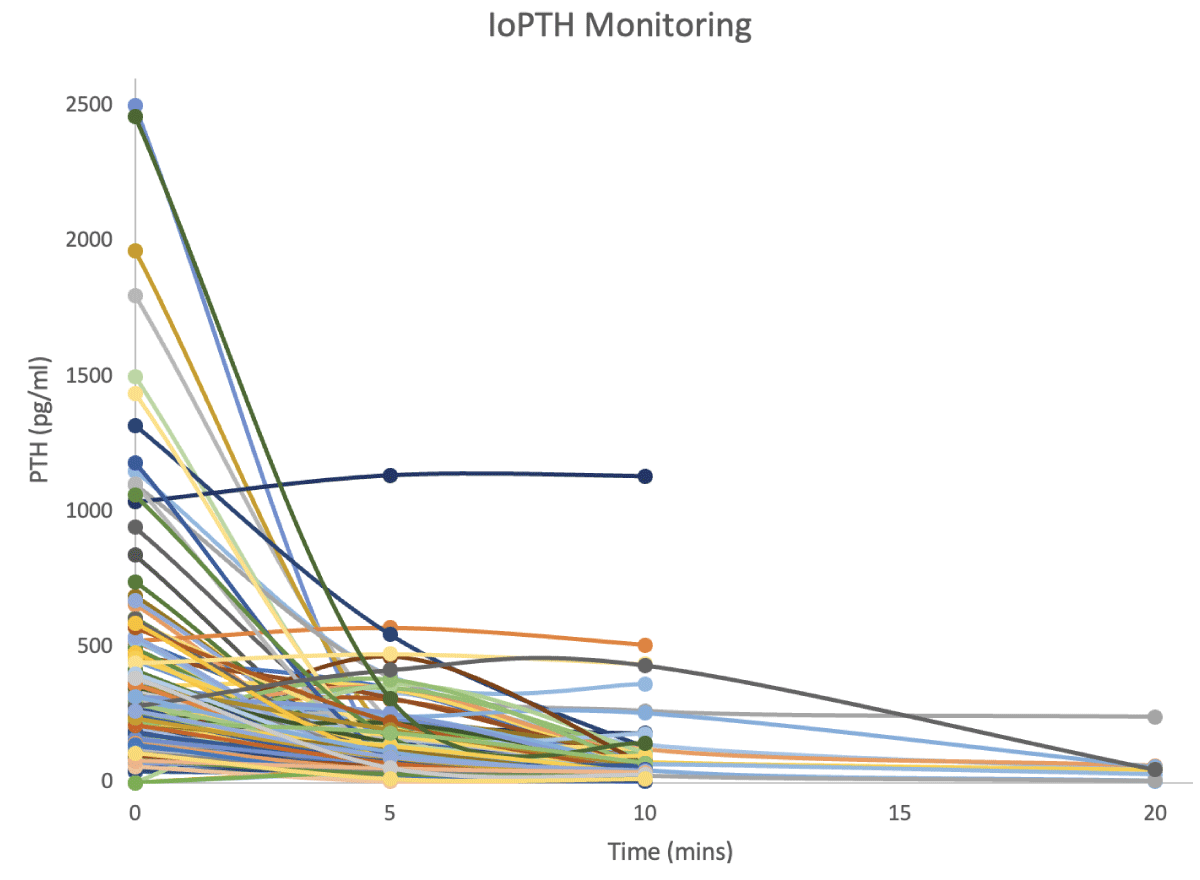
249, consecutive primary HPT patients had accurate preoperative parathyroid imaging and underwent a focused MIP (Table 1). The average cohort age was 59 ± 12 years, and 76% were female (Table 1). The mean preoperative serum calcium level was 10.9 ± 0.8 mg/dl and the median PTH was 114 pg/ml (normal < 86 pg/ml). Preoperative imaging tests were as follows: ultrasound alone 6 patients 2.4%, sestamibi scan alone 99 patients 39.8%, 4D-CT 4 patients 1.6%, and various other combinations listed in Table 1. Sestamibi scan had the highest proportion of positive imaging results when utilized alone (90%) or in combination with a 4-D CT scan (93%), significantly better than all other studies (p < 0.05). The median incision size was 3.0 cm and the mean surgery time was 90.8 minutes (range 32-253). The mean drop in ioPTH was from 250 pg/ml baseline to 58 pg/ml ten minutes after adenoma excision. MIP using ioPTH success rate was 93.4% (Table 2 and Figure 1); in 6.6% of cases ioPTH levels did not drop and procedures were converted to standard neck explorations, which were successful in all but two patients. All study participants had abnormal parathyroid glands excised. In terms of complications, 3.0% of patients had mild voice changes that recovered at a 3-month follow-up, while two patients (0.08%) had postoperative bleeding requiring reoperation.
| Table 1: Cohort Demographics, localization and surgical results. | |
| Mean Age ± SD | 60 ± 12 |
| Sex | |
| Male (%) | 62 (25) |
| Female (%) | 187 (75) |
| Median BMI (IQR) | 27.2(23-32) |
| Median (IQR) Pre-Operative PTH (pg/ml) | 114 (86-169) |
| Mean Per-operative Serum Ca2+ ± SD (mg/dL) | 10.9 ± 0.8 |
| Mean Pre-operative Ionized Ca2+± SD (mmol/L) | 1.4 ± 0.1 |
| Pre-operative Imaging | |
| U/S alone (%) | 6 (2.4) |
| Nuclear Med alone (%) | 99 (39.8) |
| 4-D CT Scan (%) | 4 (1.6) |
| U/S + Sestamibi Scan (%) | 101 (40.6) |
| U/S + 4D-CT (%) | 5 (2) |
| Sestamibi + 4D-CT (%) | 14 (5.6) |
| U/S + Nuclear Medicine + 4D-CT (%) | 20 (8) |
| Resection Location | n |
| Right Upper | 78 |
| Right Lower | 59 |
| Left Upper | 74 |
| Left Lower | 66 |
| Right Sided Adenoma | 137 |
| Left-sided Adenoma | 140 |
| Localization Success Rate by Imaging Modality | % (Corrected p - value) * |
| U/S Alone | 67% |
| Nuc Med Alone | 90% |
| CT Scan Alone | 75% |
| Nuc Med + U/S | 93% |
| CT+Nuc Med | 93% |
| CT + US | 100% |
| All 3 tests | 85% |
| Conversion from MIP to Open (%) | 8 (3.2) |
| Pre-operative Complications (%) | 1 (0.4) |
| -Difficult intubation requiring multiple attempts | |
| Intraoperative Complications (%) | 2 (0.8) |
| -Anterior Juglar Vein Hemorrhage (resolved) -Hematoma formation after ETT tube pulled |
|
| Post-Operative Complications (%) | 9 (4.7) |
| Hoarseness/Dysphagia requiring ENT laryngoscopy | 8 (3.3) |
| Hematoma | 1 (0.4%) |
| Median Length of Hospital Stay (days) | 1 |
| *Fis her Exact Test for Imaging combinations with Bonferroni Correction | |
| Table 2: Intraoperative Parathyroid Hormone (IoPTH) Monitoring results. | |
| IoPTH Monitoring (%) | n (%) |
| Yes | 244 (98) |
| No | 5 (2) |
| Intraoperative PTH (pg/ml) | Median (IQR) Mean (%) |
| Median baseline PTH | 193.55 (133-312) |
| Median immediately following excision Median PTH 10 mins post-excision |
77.1 (46-128) 26.7 (17-47) |
| Median PTH 20 mins post-excision (n = 9) | 48.4 (31-57) |
| Median IoPTH Decrease from Baseline at 20 Mins | 87% (79- 92%) |
| > 50% Drop IoPTH and within the normal range at 20 mins (%) “success” | 220 (90.6%) |
| > 50% Drop IoPTH and elevated IoPTH at 20 mins (%) | 7 (2.9 %) |
| < 50% decrease in IoPTH at 20 mins “failures” | 16 (6.6 %) |
| Failure Re-Operations (%) N = 16 | 3 (18.8 %) |
Figure 1: Drop in ioPTH level in nearly all patients following removal of a single abnormal parathyroid gland.
The Sestamibi scan was the single best preoperative localization study to identify a solitary abnormal parathyroid gland. If the sestamibi scan is positive, no other localization study is necessary. Focused MIP provided a cosmetically pleasing small incision, with a high success rate of identifying and removing an abnormal gland in a relatively short operative time, and a very low complication rate. The lateral approach to the parathyroid glands that are almost always located posterior to the thyroid facilitates parathyroid identification and excision and is easier to use than the more conventional midline approach. The midline approach does facilitate bilateral neck exploration, but this is not necessary in most patients as 93% had a successful outcome with a focused unilateral approach. Fahey, et al. [2] have demonstrated previously that limited parathyroid operations, utilizing any localizing strategy, were more cost-effective than nondirected bilateral neck explorations. Additionally, Doherty, et al. [3] estimated that total costs of re-operative parathyroid surgery were more than twice the cost of an initial operation suggesting that successful surgery provides a very important monetary result. Furthermore, two recent analyses [4-6] demonstrate higher cure rates, very low recurrence rates, and lower rates of bilateral conversion for primary HPT patients undergoing MIP with ioPTH. These results were identical to the results reported here. In summary, MIP with ioPTH provides excellent results for patients with primary hyperparathyroidism and the identification of a single abnormal gland on imaging. This will cure the disease 93% of the time. If the ioPTH levels do not drop as described above, bilateral neck exploration is indicated as a small proportion of patients will have a multi-gland disease not identified on pre-operative imaging. This is most common in the family setting of MEN-1 as those patients always have multiple abnormal parathyroid glands.
- Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, Potts JT Jr. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014 Oct;99(10):3561-9. doi: 10.1210/jc.2014-1413. Epub 2014 Aug 27. PMID: 25162665; PMCID: PMC5393490.
- Powell AC, Alexander HR, Chang R, Marx SJ, Skarulis M, Pingpank JF, Bartlett DL, Hughes M, Weinstein LS, Simonds WF, Collins MF, Shawker T, Chen CC, Reynolds J, Cochran C, Steinberg SM, Libutti SK. Reoperation for parathyroid adenoma: a contemporary experience. Surgery. 2009 Dec;146(6):1144-55. doi: 10.1016/j.surg.2009.09.015. PMID: 19958942; PMCID: PMC3467310.
- Fahy BN, Bold RJ, Beckett L, Schneider PD. Modern parathyroid surgery: a cost-benefit analysis of localizing strategies. Arch Surg. 2002 Aug;137(8):917-22; discussion 922-3. doi: 10.1001/archsurg.137.8.917. PMID: 12146990.
- Doherty GM, Weber B, Norton JA. Cost of unsuccessful surgery for primary hyperparathyroidism. Surgery. 1994 Dec;116(6):954-7; discussion 957-8. PMID: 7985102.
- Quinn AJ, Ryan ÉJ, Garry S, James DL, Boland MR, Young O, Kerin MJ, Lowery AJ. Use of Intraoperative Parathyroid Hormone in Minimally Invasive Parathyroidectomy for Primary Hyperparathyroidism: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2021 Feb 1;147(2):135-143. doi: 10.1001/jamaoto.2020.4021. PMID: 33211086; PMCID: PMC7677873.
- Ishii H, Mihai R, Watkinson JC, Kim DS. Systematic review of cure and recurrence rates following minimally invasive parathyroidectomy. BJS Open. 2018 May 28;2(6):364-370. doi: 10.1002/bjs5.77. PMID: 30511037; PMCID: PMC6254009.