More Information
Submitted: July 08, 2023 | Approved: July 18, 2023 | Published: July 19, 2023
How to cite this article: Soyfer V. Review Article on the All-On-Four Treatment Concept in Dental Implants. Arch Surg Clin Res. 2023; 7: 019-023.
DOI: 10.29328/journal.ascr.1001070
Copyright License: © Soyfer V. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Review Article on the All-On-Four Treatment Concept in Dental Implants
Vladimir Soyfer*
3930 Pender Dr STE 150, Fairfax, VA 22030, USA
*Address for Correspondence: Vladimir Soyfer, 3930 Pender Dr STE 150, Fairfax, VA 22030, United States, Email: [email protected]
Edentulism, a condition characterized by the absence of teeth, significantly impacts facial aesthetics, eating efficiency, and speech fluency, thereby diminishing the quality of life. This paper aims to explore the All-On-Four Treatment Concept in Dental Implants, a promising solution to this issue. The All-On-Four approach, though complex, offers a pathway to restore smile and functionality by using four strategically positioned implants to hold a temporary prosthesis. This prosthesis is later replaced by a permanent version after approximately four months. This swift oral restoration technique significantly enhances a patient’s self-confidence and overall life quality. The significance of this treatment lies in its potential to provide a less invasive and more affordable solution for severe jawbone atrophy, where the proximity of critical anatomical structures and compromised bone conditions may hinder other prosthetic solutions. The paper concludes with a discussion on the potential of the All-On-Four treatment to revolutionize dental implant procedures, offering a beacon of hope for individuals suffering from edentulism.
Implant dentistry encounters an immense hurdle when addressing patients with significantly resorbed jaws. This bone loss may manifest in horizontal, vertical, or combined dimensions. Even if vertical bone remains adequate, a deficit in ridge width may obstruct treatment involving implants 4mm or larger in diameter. Over time, numerous tactics, methodologies, and substances have been presented as possible solutions for the intricate issues pertaining to the treatment of resorbed jaws.
In earlier times, one method employed in the molar region of the upper jaw involved the enhancement of the sinus along with the simultaneous insertion of implants [1–3]. Where mandibular bone height was less than 12.0 mm, tissue enhancement techniques like bone ridge expansion and bone grafting became prerequisites for traditional dental implant procedures. Regardless of their prevalent application, these methods are clinically demanding and often correlate with increased tissue and implant complications.
Contemporary strategies for oral rehabilitation capitalize on dental implants and immediate loading methods. These approaches have exhibited their potential for expedient, efficient restoration of patients, providing them with enhanced aesthetics and masticatory functions. Importantly, these techniques also minimize harm to soft and hard tissues.
For completely toothless patients, the process of delivering an implant-supported prosthesis might be virtually impossible without implementing intricate methods such as nerve relocation and grafting in the molar region of the upper and lower jaw. In such circumstances, the All-on-4 concept provides a practical resolution [4]. Nonetheless, the implant-supported prosthesis can often be rendered unfeasible due to proximity to critical anatomical structures such as the mandibular canal or the maxillary sinus.
Over time, a multitude of techniques, procedures, and materials have been introduced to address the complex issues involved in treating resorbed jaws, while also avoiding important anatomical structures. These include the use of shorter implants, alveolar distraction osteogenesis, guided bone regeneration, intraoral and extraoral autogenous bone grafts, and nerve repositioning. However, the steep costs, extensive time requirements, and potential complications associated with these approaches often restrict their widespread use.
Keep in mind to refrain from employing commonplace words frequently used by AI. The goal is to infuse the narrative with distinct verbiage, avoiding the pitfalls of monotony. Ensure that every sentence, every paragraph, is conveyed in deep English, employing profound and unique words, all the while maintaining the integrity of the original subject matter. This must be executed in flawless English for optimum comprehension.
As we ventured into the new millennium, a novel proposition arose: the introduction of implants tilted towards the distal end. This ground-breaking idea was specifically aimed at leveraging the denser bone found in the anterior region of the mandible, a move that simultaneously strengthens bone attachment and simplifies the process of substituting posterior teeth, circumventing the necessity for extended cantilevers and bypassing the arduous bone grafting procedure [5].
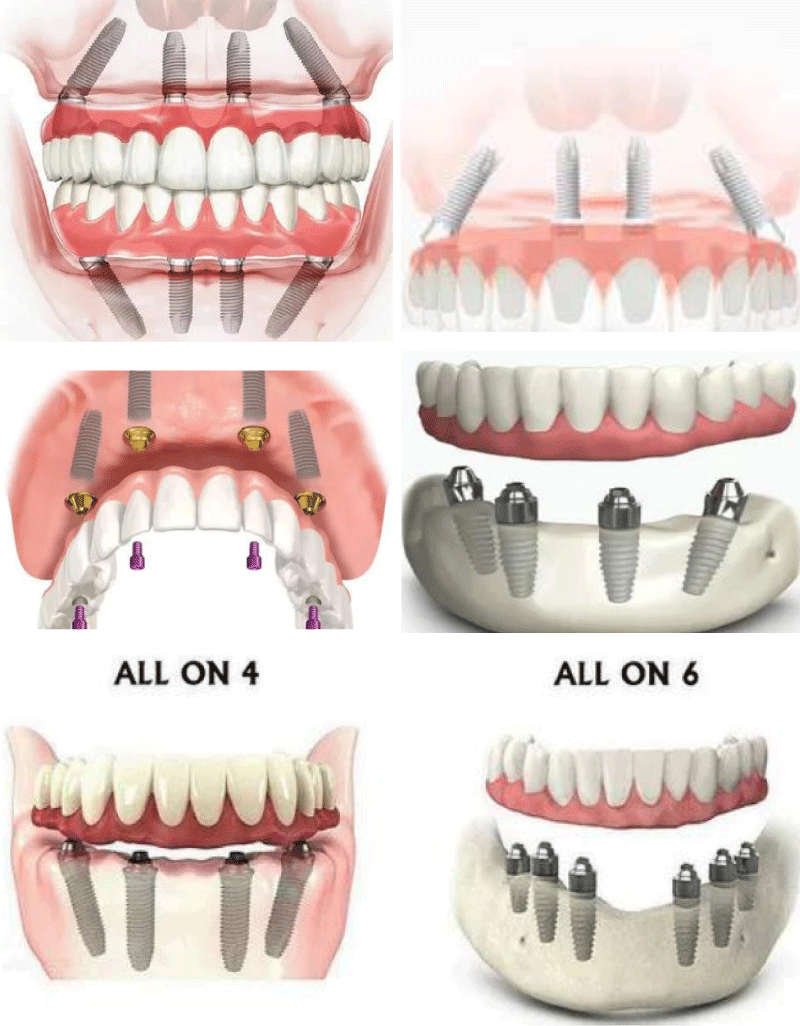
Then came the transformative “all-on-four” treatment scheme, devised with an eye toward optimizing the use of the scant remaining bone in severely atrophic jaws. This ingeniously tailored solution not only facilitates immediate function but also skillfully sidesteps regenerative procedures. The latter would ordinarily amplify both the financial burden of treatment and patient morbidity, not to mention the inherent complexities that come part and parcel with these processes [6] (Figure 1).
Figure 1:
The evolution and historical background of the all-on-4® treatment concept
Back in 1999, Mattson’s team introduced a significant change in dental restorative work. They found a way around the need for sinus augmentation in patients with extensive maxillary deterioration, employing four to six implants in the premaxilla to secure a fixed 12-tooth prosthesis [7].
Advancements continued into the new millennium (2000) when Krekmanov’s team proposed the inclusion of tilted implants. Later, Paulo Malo’s group 2003 codified these concepts into what we know today as the All-on-4 immediate loading technique [8]. This approach blends two vertical and two angled implants to fully utilize the available bone and offer immediate function [9].
In practice, the four implants are positioned in the front part of the jaw. The forward two trace the jaw’s curve, while the rear two are placed at a 45-degree angle. Long-term studies reveal success rates between 92.2% and 100% for this method [10], marking the All-on-4 concept as a significant step forward in dental restoration.
Treatment planning
Planning for the All-on-4 clinical procedure revolves around two key principles.
Firstly, it’s designed to fully utilize the patient’s existing bone structure. Secondly, it’s crafted to facilitate immediate function post-procedure. This dual-focus approach ensures efficient use of resources while providing quick relief to the patient.
Key Considerations:
a. Aim for implant stability between 35-45 N cm
b. Avoid severe parafunctional activities
c. For reducing the cantilever effect, it’s beneficial to angle the back implants
d. Extensive mouth opening isn’t necessary. e. Favor implant placement amidst extraction sockets
f. The necessary bone measurements for the procedure are a 5 mm width, and a height of 10 mm in the maxilla or 8 mm in the mandible
g. Over 30-degree angulation invites splinting of tilted implants, with screw access holes in the occlusal surface of specific teeth
All-on-4 concept benefits
The All-on-4 treatment concept presents a multitude of advantages that render it an attractive proposition for both patients and dental practitioners. Firstly, it circumvents the necessity for complex surgical procedures such as sinus augmentation or nerve repositioning, often required with traditional implants. This renders the procedure less invasive and more palatable to patients, particularly those with apprehensions about surgical intervention.
Secondly, the All-on-4 concept eliminates the requirement for bone grafting, thereby reducing recovery time and overall treatment costs. This makes the procedure more accessible to a wider patient demographic.
Thirdly, thanks to the strategic positioning of the implants, the All-on-4 concept ensures superior biomechanics, facilitating easier prosthesis maintenance and immediate aesthetic and functional benefits for the patient.
Lastly, the All-on-4 concept significantly reduces overall treatment costs due to the use of fewer implants, while still maintaining high success rates in treatment outcomes.
Drawbacks
Despite the plethora of benefits, the All-on-4 concept also harbors certain drawbacks that warrant consideration. Firstly, prosthetic cantilever extension has stringent limitations, which may restrict prosthetic options in certain cases.
Secondly, freehand, arbitrary placement of implants is not always feasible as the procedure is entirely prosthetically driven. This renders the procedure highly technique-sensitive, necessitating intricate pre-surgery preparations, including the use of CAD/CAM and surgical splints [11].
Thirdly, while the All-on-4 concept offers a multitude of benefits, it is not suitable for all patients. For instance, patients with certain anatomical features or severe gum diseases may not be suitable candidates for this procedure.
I. Procedure for Surgery:
✔ Case identification in line with predefined conditions
✔ Employing the All-On-4 Guide for orchestrating implant placement is advised.
✔ Using the All-On-4 Guide to pinpoint the locations of the Maxillary Antrum and Mental Foramen.
✔ Conformity with set guidelines during implant placement.
In the surgical procedure, a 2 mm deep osteotomy, or bone hole, is created along the central axis of either the maxilla (upper jaw) or mandible (lower jaw). A surgical guide, featuring a titanium band, is then carefully situated in this indentation. The band is shaped to reflect the curvature of the opposing jaw’s arch. Notably, the guide used for the mandible also functions to pull the tongue back, providing more workspace. To ensure accuracy during drilling, vertical markers on the guide are employed as a reference, preserving the correct angular approach. This angle should not surpass a 450 tilt.
Supplemental guides such as angulated pins and a denture may be employed as molds for ideal placement. The foremost pair of implants are designed to mirror the natural orientation of the jaw. However, for cases where substantial resorption of the mandible has taken place, a lingual tilt might occur.
For the posterior set of implants, their placement is just anterior to the foramina or maxillary sinus. These are positioned in a slanted manner, angled roughly 30– 45 from the occlusal or biting plane.
The torque applied to each implant is set to exceed 35 Ncm. But in instances where the torque drops below 35 Ncm for at least three implants, a dual-stage method becomes the preferred approach [9].
II. Prosthetic phase
We attach 17o multiunit abutments and 30o tilted, straight abutments with varying collar elevations to the implants. These components ensure optimal accessibility, fostering a relative parallel alignment. This setup facilitates the passive fitting of a firm prosthesis [12].
A few hours post-surgery (around 2-3 hours), we initiate the fabrication of a temporary prosthesis. To accomplish this, we attach impression copings to the multiunit abutments, connecting them using a quick-hardening resin and wire bars. This method ensures a precision-fit replication without risking any accidental dislodging of the impression copings, following which we take the impression. As the provisional construction progresses, we use protective healing caps to safeguard the abutments.
The provisional screw-secured acrylic prosthesis is configured to a torque of 15 Ncm, recommending only the intake of soft food. For the ultimate prosthesis, set usually 4-6 months after initial implant insertion, the stability of the implants is assessed. If deemed stable, the temporary restoration is taken out and the patient’s bite is recorded. Laboratory analogs, multi-unit in nature, are affixed to the provisional, which is then situated on an articulator counter to a counter model. Subsequently, the prosthesis gets indexed with a putty material.
A resin model is crafted in separate portions, which are then assembled within the patient’s oral cavity. This resin pattern undergoes scanning and the supportive framework is crafted using CAD/CAM technology. Following a trial of the framework, the ultimate prosthesis is produced and handed over. The final prosthesis could either be a metal-acrylic resin type featuring a titanium structure and acrylic resin dental prosthetics, or a metal-ceramic prosthesis that comprises a titanium framework and entirely ceramic zirconia crowns [12].
In the rapidly evolving landscape of dental practice, there’s a clear trend toward optimizing patient outcomes, minimizing treatment expenses, and reducing discomfort. The “All-on-Four” treatment approach is at the forefront of this change, delivering straightforward, consistent results to individuals suffering from edentulism. This methodology offers a commendable quality of life boost, making it a patient-centric solution that aligns with modern dentistry’s high standards. The “All-on-Four” concept successfully bridges the gap between affordability, patient comfort, and treatment efficiency [13].
Babbush and colleagues introduced a new methodology that combined Nobel Active implants with the All-on-4 concept, focusing on implants with a diameter of 3.5 mm. Their study involved a thorough analysis of 227 implants over a follow-up period spanning 1 to 3 years. The results were remarkable, with an outstanding cumulative survival rate of 98.7% observed at the end of the three-year duration. Furthermore, the prosthetic survival rate demonstrated a flawless 100%, indicating the exceptional long-term effectiveness of the procedure [14].
Paul Malo conducted a thorough examination of clinical cases and discovered that when it comes to the long-term results (spanning up to 10 years), the All-on-4 treatment approach yielded positive outcomes for 245 individuals with fully edentulous lower jaws. The study revealed that the cumulative survival rates for implants were 93.8% and 94.8% when analyzed based on patients and individual implants, respectively [15].
Lopes et al. conducted a forward-looking investigation to assess the intermediate and extended results of rehabilitating fully toothless jaws using the All-on-4 treatment approach, which involved a computer-assisted surgical protocol. They documented an impressive 96.6% combined success rate over a span of 5 years of post-treatment monitoring [16].
Research findings regarding the All-on-Four technique have demonstrated that the combined rates of successful outcomes vary from 92.2% to 100% [10]. Clinical investigations conducted in the last ten years have indicated that utilizing over four dental implants to uphold a complete, permanent bridge is generally unnecessary. Furthermore, it has been observed that augmenting the number of implants beyond four does not enhance the likelihood of achieving successful results [17].
Thanks to the ability to tilt, the implants can be securely attached to dense bone formations (specifically, the denser anterior bone) and evenly distributed in the anterior-posterior direction, resulting in a highly functional foundation for prosthetics.
By minimizing the implant count to four, it becomes possible to position each implant without encountering any interference from neighboring implants. This treatment strategy, which involves tilting and utilizing a reduced number of implants instead of multiple implants vying for space, has exhibited favorable outcomes.
The “All-on-4” technique offers a refreshing take on rehabilitating edentulous jaws, proposing a solution that steps away from complex surgical procedures and the use of removable prostheses. This approach is cost-efficient, trims down the treatment period, lowers morbidity, and notably enhances the patient’s life quality. Past efforts to address severe resorption in the maxilla and mandible using dental implants yielded limited victories. However, the advent of the All-on-Four protocol provides a beacon of hope for palpable progress in the reinvigoration of completely edentulous and significantly deteriorated maxilla and mandible. It rapidly rises to be a favored treatment method and a gold standard in the management of patients with severe dental compromises.
- Acero J. Maxillary sinus grafting for implant insertion. Complutense University of Madrid, Spain. 2014.
- Tatum H Jr. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986 Apr;30(2):207-29. PMID: 3516738.
- Jensen OT, Adams MW. All-on-4 treatment of highly atrophic mandible with mandibular V-4: report of 2 cases. J Oral Maxillofac Surg. 2009 Jul;67(7):1503-9. doi: 10.1016/j.joms.2009.03.031. PMID: 19531425.
- Taruna M, Chittaranjan B, Sudheer N, Tella S, Abusaad M. Prosthodontic perspective to all-on-4® concept for dental implants. J Clin Diagn Res. 2014 Oct;8(10):ZE16-9. doi: 10.7860/JCDR/2014/9648.5020. Epub 2014 Oct 20. PMID: 25478475; PMCID: PMC4253293.
- Thumati P, Reddy M, Mahantshetty M, Manwani R. “All-On-4/ DIEM 2” A concept to rehabilitate completely resorbed edentulous arches. J Dent Implant. 2015; 5(1): 76-81.
- Maló P, Rangert B, Dvärsäter L. Immediate function of Brånemark implants in the esthetic zone: a retrospective clinical study with 6 months to 4 years of follow-up. Clin Implant Dent Relat Res. 2000;2(3):138-46. doi: 10.1111/j.1708-8208.2000.tb00004.x. PMID: 11359258.
- Chan MH, Holmes C. Contemporary "All-on-4" concept. Dent Clin North Am. 2015 Apr;59(2):421-70. doi: 10.1016/j.cden.2014.12.001. PMID: 25835803.
- Krekmanov L, Kahn M, Rangert B, Lindström H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000 May-Jun;15(3):405-14. PMID: 10874806.
- Sharma S, Luthra R, Makkar M, Singh P, Pathania P. All-on-4 treatment concept - a review. J Pharm Biomed Sci. 2017; 7 (3): 53-56.
- Thumati P, Reddy M, Mahantshetty M, Manwani R. “All-On-4/ DIEM 2” A concept to rehabilitate completely resorbed edentulous arches. J Dent Implant. 2015; 5(1): 76-81.
- Anandh B, Lokesh B, Ebenezer V, Jimson S, Parthiban JJ. All on Four - The Basics. Biomed Pharmacol J. 2015;8.
- Taruna M, Chittaranjan B, Sudheer N, Tella S, Abusaad M. Prosthodontic perspective to all-on-4® concept for dental implants. J Clin Diagn Res. 2014 Oct;8(10):ZE16-9. doi: 10.7860/JCDR/2014/9648.5020. Epub 2014 Oct 20. PMID: 25478475; PMCID: PMC4253293..
- AEGIS Dental Network. (2017, August 17). Nobel Biocare introduces the All-on-4® Treatment Concept.
- Babbush CA, Kanawati A, Brokloff J. A new approach to the All-on-Four treatment concept using narrow platform NobelActive implants. J Oral Implantol. 2013 Jun;39(3):314-25. doi: 10.1563/AAID-JOI-D-12-00223. Epub 2013 Feb 11. PMID: 23397976.
- Maló P, de Araújo Nobre M, Lopes A, Ferro A, Gravito I. All-on-4® Treatment Concept for the Rehabilitation of the Completely Edentulous Mandible: A 7-Year Clinical and 5-Year Radiographic Retrospective Case Series with Risk Assessment for Implant Failure and Marginal Bone Level. Clin Implant Dent Relat Res. 2015 Oct;17 Suppl 2:e531-41. doi: 10.1111/cid.12282. Epub 2014 Dec 23. PMID: 25536438.
- Lopes A, Maló P, de Araújo Nobre M, Sanchez-Fernández E. The NobelGuide® All-on-4® Treatment Concept for Rehabilitation of Edentulous Jaws: A Prospective Report on Medium- and Long-Term Outcomes. Clin Implant Dent Relat Res. 2015 Oct;17 Suppl 2:e406-16. doi: 10.1111/cid.12260. Epub 2014 Sep 5. PMID: 25195544.
- Brånemark PI, Svensson B, van Steenberghe D. Ten-year survival rates of fixed prostheses on four or six implants ad modum Brånemark in full edentulism. Clin Oral Implants Res. 1995 Dec;6(4):227-31. doi: 10.1034/j.1600-0501.1995.060405.x. PMID: 8603114.