More Information
Submitted: December 06, 2023 | Approved: December 18, 2023 | Published: December 19, 2023
How to cite this article: Shapovalov KA, Shapovalova LA. Lecture: "First Aid to the Population in Case of Thermal Burns during Accidents, Catastrophes, Natural Disasters and Terrorist Attacks" of the Subject "Life Safety" for Humanitarian and Technical Universities. Arch Surg Clin Res. 2023; 7: 052-059.
DOI: 10.29328/journal.ascr.1001074
Copyright License: © Shapovalov KA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Thermal burns; First aid; Emergency situations; Didactics
Lecture: "First Aid to the Population in Case of Thermal Burns during Accidents, Catastrophes, Natural Disasters and Terrorist Attacks" of the Subject "Life Safety" for Humanitarian and Technical Universities
Shapovalov KA1,2* and Shapovalova LA1
and Shapovalova LA1
1State Educational Institution of Additional Pedagogical Education "Komi Republican Institute for the Development of Education", Syktyvkar, Komi Republic, Russian Federation
2State Budgetary Health Institution of the Republic of Komi "Syktyvkar Children's Polyclinic No. 3", Syktyvkar, Komi Republic, Russian Federation
*Address for Correspondence: Shapovalov KA, MD, Professor, State Educational Institution of Additional Pedagogical Education "Komi Republican Institute for the Development of Education", Syktyvkar, Komi Republic, Russian Federation, Email: [email protected]
To prepare the population to provide first aid for thermal burns in emergency situations, algorithms for modern didactics of the educational topic “Thermal burns” are proposed. The following educational issues are highlighted: 1) Local exposure to high temperature. Burns. Kinds. Classification according to the depth of the lesion; 2) Rules for determining the area of burns; 3) Signs of thermal burns; 4) The concept of burn disease; 5) First (pre-hospital emergency) aid to burnt people; 6). Domestic burns from boiling water; 7) Features of burns in children; 8) Treatment of burns; 9) Prevention of thermal burns.
Study questions
1. Local exposure to high temperature. Burns. Kinds. Classification according to the depth of the lesion.
2. Rules for determining the area of burns.
3. Signs of thermal burns.
4. The concept of burn disease.
5. First (pre-hospital emergency) aid to burnt people.
6. Domestic burns from boiling water.
7. Features of burns in children.
8. Treatment of burns.
9. Prevention of thermal burns.
Prevalence of burns [1-3]: According to statistics from the World Health Organization (WHO), burns are the 4th most common type of injury, following road traffic accidents, falls and violence. In the world, more than 6 million people annually seek medical help for burns; in 180,000 cases, burn injury ends in death. Mortality from burns per 1000 population in the United States of America (USA) ranges from 3.9 to 4.5, in Europe this figure ranges from 2.8 to 35.4, and in Southeast Asia reaches a maximum of 184.0. In India, more than 1,000,000 people suffer moderate to severe burns every year.
✔ In Bangladesh, about 173,000 children suffer moderate or severe burns every year.
✔ In Bangladesh, Egypt, Colombia, and Pakistan, 17% of child burn victims have temporary and 18% permanent disabilities.
✔ Burns are the second leading injury in rural Nepal, accounting for 5% of disability cases.
✔ In 2008, more than 410,000 burn injuries occurred in the United States, of which approximately 40,000 required hospitalization.
In the Russian Federation (RF), thermal burns occupy third place among other injuries [4]. According to Rosstat (2010), 313,500 cases of burn injury were registered in the RF [5]. About 100 thousand victims of thermal injuries are treated annually in a burn hospital, of which 40.0% - 46.0% are for deep burns. In 15.0% - 17.0% of cases, the area of IIIB-IV degree burns in patients exceeds 20.0%. In-hospital mortality for deep body burns is approximately 8.7%, and the average bed turnover for the treatment of burn patients is 11.9 [6].
Risk factors occurrence of burns [1,7,8]:
1) Activities that increase the likelihood of exposure to fire sources;
2) Poverty, overcrowding, and lack of adequate safety measures among the population;
3) Young girls performing household duties such as cooking and caring for small children;
4) Presence of underlying diseases, including epilepsy, peripheral neuropathy, as well as physical and cognitive disability;
5) Excessive drinking and smoking by both adults and children;
6) Unimpeded access to flammable, combustible, and chemical substances that can be used as a means of aggression (in particular, acids);
7) Use of kerosene as fuel for non-electric household appliances;
8) Failure to comply with safety rules when using liquefied petroleum gas and electricity.
Local exposure to high temperature [9-13]: A burn is tissue damage caused by heat, electric current, chemicals, or radiation. Accordingly, burns are distinguished:
- thermal;
- electric;
- chemical;
- radiation (ray);
- combined.
Thermal burns in relation to the total number of injuries at home and at work in peacetime range from 5.0 to 12.0%. They arise as a result of exposure to high external temperatures of flames, hot gases, boiling and burning liquids, and solid objects. Tissue damage during burns is greater the higher the temperature and the longer its effect.
The degree of damage from burns also depends on:
- area;
- localization;
- physical properties of the thermal agent (flame, hot steam, molten metal, hot sticky and viscous liquids).
Classification of burns by depth of injury [14-16]:
Surface:
I degree sunburn ~90.0% - 95.0% of the entire body surface.
I degree - severe redness (hyperemia) and swelling of the skin
I degree sunburn ~90.0% - 95.0% of the entire body surface
II degree – detachment of the epidermis and the formation of blisters with light yellow liquid.
II-degree burn on the left wrist. Detachment of the epidermis with the formation of a tense bubble with light yellow liquid
II-degree burn of the right shoulder, forearm, and wrist. Detachment of the epidermis in all segments of the right upper limb with the formation of multiple blisters with light yellow liquid
III A degree – of necrosis of the superficial layers of the skin with the formation of large tense blisters. In this case, the germinal (papillary or germinal) layer of the dermis is partially damaged. Scab formation is possible.
Superficial burns heal on their own. With degree IIIA, epithelization is possible due to preserved skin appendages (sebaceous and sweat glands, hair follicles) and remnants of the germ layer.
III A degree burn on the posterior outer surface of the right foot
III A degree burn
Deep:
III B degree - damage to the entire germ layer of the skin. Bubbles with bloody contents, their bottom is whitish in color. The sensitivity of the burned areas is reduced or absent. Scab formation is possible.
IV degree - necrosis of tissues located deeper than the skin itself with damage to blood vessels, nerves, muscles, and bones. Sometimes the formation of a scab or charring of the burned surface.
IV-degree burn of the left leg and foot with elements of soft tissue necrosis and mummification of areas of the toes
Deep burns cannot heal on their own. They require plastic surgery (skin grafts) and long-term treatment.
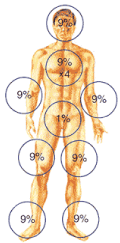
To determine the area of burns, the following are used [17-19]:
“Rule of nine”: The entire surface of an adult’s body is divided into areas that are multiples of 9% in area:
Head, neck – 9%.
Upper limbs – 9% each:
- left – 9%;
- right – 9%.
Torso – 36%, including:
- anterior surface of the body – 18%;
- of which the anterior surface of the chest – 9%;
- belly – 9%;
- posterior surface of the body – 18%;
- of which the posterior surface of the chest is 9%;
- lumbar region, buttocks – 9%.
Lower extremities – 18% each:
- left – 18%;
- right – 18%;
- incl. thigh – 9%;
- lower leg, foot – 9%.
Perineum – 1%.
Total: 100%.
Schematic representation of rule "9"
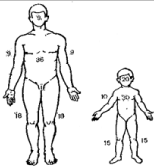
The “rule of five” is used in children under 5 years of age: the entire surface of the body of a child under 5 years of age is conditionally divided into areas that are multiples of 5% in area:
Head, neck – 20%.
Torso – 30%.
Upper limbs – 10%.
Lower extremities – 15% each.
Total: 100%.
Schematic representation of rule "5"
The “palm” rule: The palm area of an injured adult is approximately equal to 1% of the surface of his body.
Schematic representation of the palm rule
Other methods determining the area of burns (B.N. Postnikov, N.N. Blokhin, Yu.Yu. Dzhanelidze, G.D. Vilyavin) [20-22]:
According to B.N. The postnic area is measured by placing a sterile transparent film on the burning surface, on which the contours of the burn are drawn in ink, after which the film is applied to graph paper, the burn area is calculated in square centimeters and calculated as a percentage of the total body surface, taking it as 16,000 cm2.
Proposed by N.N. Blokhin’s method for calculating the percentage of burns to the body area, taking into account the patient’s height, is more advanced. Based on the coincidence of height figures on average 150–180 cm and the surface of the skin, which varies from 15,000 to 18,000 cm2, the author believes that the height figure can be conditionally taken as 1% of the surface of the human skin. For example, with a burn of 1,500 cm2 in a patient 170 cm tall, the relative burn area will be 1,500: 170 = 8.8%.
The disadvantage of all the proposed methods for measuring and documenting burns is that they do not provide qualitative characteristics of the degree and location of burns.
More accurate is the formula proposed by Yu.Yu. Dzhanelidze, when the diagnosis is recorded as a fraction: the numerator indicates the percentage of damage, and the denominator indicates the degree of burn. For example: 12.0% with an additional listing of the location of the lesion, II and III degrees (chest, face, etc.).
However, it should be emphasized that the method of documentation of burns should not only determine the size and percentage of the lesion but also reflect its extent and location: it should be simple to use in all conditions, especially with mass casualties.
To measure the burn area according to G.D. Vilyavin needs special forms with body silhouettes printed on them against a background of graphed squares and a table. The silhouettes are shaded with colored pencils, and the area is calculated using the table.
The last four listed methods are usually used by doctors in surgical hospitals and specialized burn centers.
Signs of manifestations of burns: Local and general manifestations of burns depend on the depth and area of the lesion. Superficial burns that are small in area (5.0% - 7.0%) are classified as outpatient and may result in pain of varying intensity, increased heart rate, and an increase in body temperature of 1 ºC - 2 ºC.
Extensive superficial and deep burns are accompanied by the development of burn disease: During this disease there are periods:
- burn shock;
- acute burn toxemia;
- burn septicotoxemia;
- recovery.
The severity of burn disease depends mainly on the area, degree, and location of the damage. Victims with severe burns and signs of burn disease are subject to hospital treatment. The prognosis for burn healing is determined by the depth of tissue necrosis and the thickness of the skin in the area of damage.
First aid (FA) for the burned person [23-25]:
1) Stop the effect of the damaging factor - quickly remove burning clothing, pour water on the burning surface, and use snow, sand, and clay for these purposes. Throw a blanket, coat, carpet, or tarp over the victim, remembering that pressing burning clothing to the skin increases the effect of high temperature and leads to a deepening of the burn. If a victim is covered with his head during a prolonged burning of clothing, then damage to the respiratory tract from hot air, smoke, and carbon monoxide poisoning may occur. Therefore, air access to the upper respiratory tract is not blocked. There is no need to force the victim to breathe carbon monoxide and other toxic combustion products.
2) After the burning stops, the loose remains of smoldering clothing are removed, and the stuck ones - in order to avoid further traumatization of the affected area - are not touched. There is no need to try to clean the burn surface from deeply embedded foreign elements at the scene of the incident. The affected areas are cooled by applying fabrics (towels, scarves, napkins) moistened every 3 minutes - 5 minutes with cold water or applying dry cold (plastic bags or bubbles filled with ice or snow) to the burned surface of the body. Cooling reduces pain and prevents swelling and keeps the area of thermal damage minimal and should be done within 10 to 15 minutes after the burn. In the cold season, the patient must not be allowed to become hypothermic. Severe pain is one of the main reasons for the deterioration of the general condition of the victim in the first hours after a burn. It can significantly worsen the victim's condition. To relieve pain, it is recommended to use available painkillers: amidopyrine, analgin, acetylsalicylic acid in combination with diphenhydramine or suprastin.
3) After cooling, a dry bandage of bandages or gauze is applied to the burned surface, the patient is given plenty of fluids up to 1.0 liters - 1.5 liters (tea or coffee, mineral water) and sent to a medical institution. Immediately applying bandages with medications is not recommended, because at the scene of the incident, it is not possible to fully clean the burn wound, and an applied ointment bandage and, especially, with dyes can mask local changes in the burn surface and disorient doctors at subsequent stages of treatment. In addition, ointment dressings prevent the formation of a dry scab and often contribute to the spread of purulent infection.
4) The affected limbs are immobilized with standard or improvised splints. It is necessary to ensure non-traumatic and painless transportation and warming of the victim. If there is a long transportation ahead, the victims are given water or a salt-alkaline mixture to drink: 1/2 teaspoon of sodium bicarbonate (baking soda) and 1 teaspoon of sodium chloride (table salt) per 1 liter of water. In case of mass casualties and in case of transportation, a special card is filled out for each victim indicating the circumstances of the burn and the measures taken. In case of thermal skin burns (except for limited first-degree burns), you should call a doctor or immediately take the victim to the nearest medical facility.
5) For thermal burns of II and III degrees, do not wet the burned areas with cold water. As part of first aid, it is also not allowed to wash severe burns with ethyl alcohol, hydrogen peroxide, lubricate with ointments, fats and oils, sprinkle with baking soda, starch or other “folk” remedies. Treating burns with ointments or applying compresses should only be done by qualified medical professionals.
6) In case of deep, extensive burns, the victims are urgently evacuated to the nearest surgical hospital. When providing PN to patients with thermal injuries, attention should be paid to and promptly diagnosing respiratory tract burns in victims. They are most often caused by an open flame, as well as inhalation of hot air, steam, or smoke. Early diagnosis of respiratory tract burns should be based on a thorough analysis of the circumstances of the burn injury. If a burn to the face, nose, lips, tongue, neck occurred in a closed room due to a fire, then there is every reason to suspect damage to the respiratory tract. Hoarseness, sore throat, difficulty breathing, sore throat when swallowing, dry cough, shortness of breath and other clinical signs of respiratory tract burns are indications for emergency hospitalization of the patient.
When a skin burn and a burn of the respiratory tract are combined, burn shock can occur with a lesion area half as large as with a skin burn alone.
Domestic burns with boiling water (These also include injury resulting from contact with hot steam) [26-27]:
Such injuries occur when a limb unintentionally falls into a container of very hot liquid or when boiling liquid accidentally comes into contact with the body. Burns from boiling water usually do not lead to serious consequences, and treatment often proceeds favorably. In this case, the degree of damage is characterized by the same four degrees in accordance with the accepted classification, and each specific case depends on the following characteristics of the boiling liquid: 1) Speed and pressure; 2) The volume of liquid and the area of its contact with the victim’s body; 3) Time of contact with skin; 4) Temperature and chemical composition; 5) Anatomical and physiological features of the structure of a specific burned area of the body.
I degree boiling water burn
It has been established that a burn from pure boiling water causes less consequences than exposure to homemade syrups or brines. In such cases, in adults, the hands and forearms are most often affected, less often - the thighs, legs, abdomen, feet and chest.
Features of burns in children: Body burns in children are among the most common, often severe, mechanical injuries of soft tissue and are caused by exposure to high temperature or chemicals. About 20% of children's domestic injuries requiring hospital treatment are burns. The most common traumatic agents are hot liquids (water, soup, milk); Burns from flames or heated objects are less common. Chemical burns in children are rare.
The child played with flammable substances
Among those burned, children under 3 years of age predominate, who, due to the carelessness of adults, accidentally sit in a vessel with hot water or tip it over themselves. Therefore, the typical localization in the first case is the buttocks, back, genitals and back of the thigh, and in the second - the head, face, neck, chest, abdomen and upper limbs. The temperature of the liquid may not often be very high, but this is quite enough to cause a 1st or 2nd degree burn on the delicate skin of a small child.
I want to touch a hot toys
With a minor burn, the child energetically reacts to the pain by crying and screaming. On the contrary, with extensive burns to the body, the child’s general condition may be severe, but despite this, he is striking in his calmness. The child is pale and apathetic. Consciousness is completely preserved. Blueness of the skin, small and rapid pulse, cold extremities and thirst are symptoms of a severe burn, indicating the presence of shock. In some cases, vomiting occurs, which indicates an even greater severity of the damage.
Prevention
When bathing small children in the bath, be sure to use a thermometer. It is necessary to check the temperature of the water before lowering the child’s body with your own elbow. He will never let you down. You cannot wash your child with “warm” tap water, as a sharp temperature change is possible (from “hot” to “boiling water”).
When feeding, you must not: 1) Carry a container with heated food over the child; 2) Place a vessel with hot liquid (teapot, coffee pot, cups of milk or jelly) on the edge of the table. It is possible that a child may accidentally knock over these items. Hot dishes should be placed in the center of the table so that the child cannot reach them [19].
Treatment of burns: begins with complex anti-burn therapy, in which the leading place is occupied by: transfusion of liquids, plasma or protein substitutes, and canned blood. At the same time, intensive antibiotic therapy is started.
During the initial treatment of the burn surface, it is necessary to clean and wash the surface of the skin around the burn, remove foreign bodies and scraps of epidermis. Large blisters are opened at the base and emptied. After drying, sterile wet-dry dressings with a 2% novocaine solution are applied to the surface of the burn, and then antiseptics (furatsilin, rivanol or a combination of alcohol and furatsilin) and syntomycin emulsion. All burn victims should be given tetanus toxoid [10,27].
Self-healing second degree burns of the neck, anterior chest and left shoulder. Late appeal
A burn wound is always primarily infected. With deep burns, the skin loses its barrier function, and dead tissue serves as a favorable environment for the development of pyogenic microflora. Therefore, when treating burns in order to prevent infectious complications, it is necessary to use widely used antibiotics in wet-dry dressings, subject to careful monitoring of the burn wound during dressings.
Currently, the main method of treating burns is a closed method. The open method is more often used for burns of the face and perineum, as well as in the treatment of infants.
The most important part of modern treatment is skin grafting, the use of which has significantly improved functional and cosmetic results, and most importantly, reduced mortality in cases of extensive burns.
To accelerate the rejection of dead tissue, proteolytic enzymes and staged excision of dead tissue during dressings are used. For closed burn wounds the following is used:
- Free skin grafting according to Thiersch;
- Gabarro’s “postage stamp” method.
Burn prevention strategies are aimed at eliminating the risk of specific types of burn injuries, outreach to populations at risk of burns, and training citizens in first aid [1,2,20,28,29]:
✔ Raising awareness;
✔ Developing and monitoring the implementation of effective policies;
✔ Studying the burden of burns and identifying risk factors;
✔ Identification of research priorities and promotion of effective methods;
✔ Implementation of burn prevention programs;
✔ Improving the quality of medical care for burns;
✔ Strengthen capacity to perform all the above tasks.
They have to:
1) Protect sources of fire and limit the height of open flames at home;
2) Promote the development and installation of cookstoves of safer design and the use of less hazardous fuels, and also explain the need to wear loose clothing when using them;
3) Encourage the development and use of non-flammable aprons for use when cooking over open flames or kerosene stoves;
4) Improve the design of cook stoves, especially in terms of their stability and inaccessibility to children;
I want to help my mother
5) Observe safety rules when handling household appliances and materials and facilitate fire safety inspections in residential premises;
6) Reduce the temperature of tap hot water;
7) Promote fire safety education and the use of smoke detectors, fire sprinklers, and emergency exit and stair systems, especially in multi-story high-rise buildings;
8) Promote the implementation and compliance of industrial fire safety requirements and use non-flammable fabrics for the production of children's nightwear;
9) Do not smoke in bed and use childproof lighters;
10) Promote the adoption of legislative requirements for the production of fireproof cigarettes;
11) Increase the effectiveness of epilepsy treatment, especially in developing countries;
12) Promote the further development of mechanisms for providing first and specialized medical care for burns, including training of medical specialists in methods of triage and management of burn patients.
Education and preparation of the population to provide first aid for thermal burns is an important stage in eliminating the severe consequences of one of the mass types of injuries during accidents, disasters, natural disasters and terrorist attacks.
A competent assessment of the victim’s condition and proper provision of first aid can significantly change the quality of medical care, speed up the recovery and rehabilitation processes of people with burns, and reduce the social costs of society.
Awareness and practical skills in studying the subject “Life Safety” of the population in combination with state control of fire safety measures and the implementation of burn prevention programs will make it possible to achieve a significant breakthrough in reducing the negative consequences of thermal burns.
The authors express their sincere love to their parents. The authors are grateful to Bychikhin N.P., Kucherenko V.Z., Zhuravlev S.M., Novikov P.E., Orlov G.A., Dobrodeeva L.K., Klepikova R.A., Udalova L.S., Lus E.A., Kuznetsova M.N., Smolnikov L.A., Ternovsky L.N., Batygina N.I., Rzhevskaya V.N., Duberman L.B., Akhmeev V.N., Schumacher R.E., Gribanov V.V., as well as all anonymous reviewers for their support, valuable advice and useful comments.
A number of photographs, drawings and diagrams, which are freely available on the Internet without indicating the authors, were used in the article in the original and in translation for scientific, informational and educational purposes, as well as to reveal the creative intent of the authors of legally published works to the extent justified by the purpose of citation.
- Burns. https://www.who.int/ru/news-room/fact-sheets/detail/burns (accessed 05.12.2023).
- Smolle C, Cambiaso-Daniel J, Forbes AA, Wurzer P, Hundeshagen G, Branski LK, Huss F, Kamolz LP. Recent trends in burn epidemiology worldwide: A systematic review. Burns. 2017 Mar;43(2):249-257. doi: 10.1016/j.burns.2016.08.013. Epub 2016 Sep 3. PMID: 27600982; PMCID: PMC5616188.
- Unizhaeva AYu, Martynchik SA. Medical and economic assessment of the costs and quality of inpatient care for burn injury. Social Aspects of Population Health 2012;(6):1-8.
- Ponomareva NA, Vorobyev AV, Zhegalov VA, Peretyagin SN. The history and stages of development of conbustiological service in Russia. Zdravookhraneniye Rossiyskoy Federatsii 2009;(6):45-48.
- Demographic Yearbook of Russia. Statistical Bulletin. Moscow: Rosstat. 2010;1-525.
- Zinovyev YeV. The ways to improve health care with extensive deep burns to the population living out of regional administrative centers. PhD. Thesis. N. Novgorod. 2008; 1-39.
- Shapovalov KA, Shapovalova LA. Self-interacting and First Aid for injuries and accidents: a tutorial. Syktyvkar, Syktyvkar State University. 1995; 20-22.
- Thermal Burns. A Practical Guide for Low-Resource Settings. https://ewma.org/fileadmin/user_upload/EWMA.org/Ukraine/Thermal_burns_-_practical_recommendation_for_resource-limited_setting__RU_.pdf
- Shapovalov KA, Shapovalova LA. Thermal destruction. Electrical burns. Thermal and radiation burns. Frostbite: lecture. Syktyvkar, Komi State Pedagogical Institute. 1995;1-4.
- Loginov LP. Modern principles of local treatment of thermal burns. Russian Med J. 2001; 9(3):123-126.
- Ariev TYa. Burns and frostbite. Medicine. 1971.
- Shapovalov KA. Meditsinskaia pomoshch' pri ozhogovoĭ travme na sudakh severnogo basseĭna [Medical care in burn injuries on board ships of the northern basin]. Voen Med Zh. 1989 Dec;(12):55-6. Russian. PMID: 2631416.
- Shapovalov KA. The organization of work of the ship's doctor. Zdravoohr Ros Fed. 1990;(10):15-19.
- Shapovalov KA, Shapovalova LA. Fundamentals of Safety of Life: Safety and security of the population in emergency situations; self-interacting and first aid for injuries and accidents: tutorial. 2nd ed., Revised and enlarged. Syktyvkar, Komi State Pedagogical Institute. 2002;122-125.
- Buyanov VM. First aid. M. 2000.
- Shapovalov KA, Shapovalova LA. First aid for thermal damage to victims during accidents, catastrophes, natural disasters and terrorist attacks. Geneva, World Health Organization, Pubrights. 2018 Apr 18:1-43.
- Shapovalov KA, Shapovalova LA. Fundamentals of Safety of Life: Safety and security of the population in emergency situations; self-interacting and first aid for injuries and accidents: a tutorial. 3rd edition, revised. and enlarged., CD. Syktyvkar, Komi State Pedagogical Institute. 2003:155-158.
- Shapovalov KA, Shapovalova LA. Types of thermal destruction. Electrical burns. Thermal and radiation burns. Frostbite: Lecture. Syktyvkar, Komi Republican Institute for Educational Development. 2015;1-10.
- Shapovalov КА, Shapovalova LA. Thermal burns. Features of didactics of teaching first aid for children, schoolchildren and adolescents. Children's medicine of the North-West (Detskaya medicina Severo-Zapada). Materials of the V National Congress with international participation "Healthy children - the future of the country. 2021;9(1):393-396. https://gpmu.org/userfiles/file/%D0%9A%D0%9E%D0%9D%D0%93%D0%A0%D0%95%D0%A1%D0%A1/2021/det_med_2021_1.pdf
- Shapovalov KA, Shapovalova LA. Fundamentals of Safety of Life: Safety and security of the population in emergency situations; self-interacting and first aid for injuries and accidents: manual. 4th ed., revised and enlarged. (Recommended by the Presidium of the Council of Educational Methodological Association of Russian universities in the field of teacher education as a textbook for students of higher educational institutions, students majoring on discipline 033300 "Safety" (09.03.2004. Protocol number 2). Syktyvkar. 2004:126-129.
- Vikhriev BS, Burmistrov VM. Burns L. Medicine. 1986.
- Atyasov NI. System of active surgical treatment of severely burned patients. Gorky: Volgo-Vyat., book. Iz-vo, 1972.
- Shapovalov KA, Shapovalova LA. Bases of didactics of an educational theme «Training of the population to first-aid treatment at thermal defeats, electric, thermal and beam burns, freezing injuries in the conditions of emergency situations». Bezopasnost' Zhiznedeyatel'nosti. 2015 Apr; (4)172: 67-69. http://novtex.ru/bjd/bgd2015/annot04.html#12
- Shapovalov KA, Shapovalova LA. Basics of Rendering First Medical Aid: Thermal Lesions. Syktyvkar, Komi Republican Institute for Educational Development. 2016; 6-11.
- Zhernov AA. Thermal burn: first aid and treatment. https://burnclinic.com.ua/termicheskiy-ozhog-pervaya-pomosch-i-lechenie
- Shapovalov KA, Shapovalova LA. First Aid for Citizens in Conditions Threatening Life and Health. Thermal burns. Syktyvkar: Komi Republican Institute of Development of Education. 2017; 1-6.
- Shapovalov KA, Shapovalova LA. Distance Learning Course "First Aid for Injuries and Accidents": Burns and Frostbite. Syktyvkar, Komi Republican Institute for Educational Development. 2017; 7-11.
- Shapovalov KA. Methodological approaches to teaching academic theme "Burns" subject "First aid for injuries suffered during accidents" for humanitarian and technical universities. WCICT 2017 WOUND CARE from Innovations to Clinical Trials. Manchester. United Kingdom. Abstracts No. 1012. 20-21 June 2017.
- Shapovalov KA, Shapovalova LA. Training the population in first aid for thermal burns during accidents, disasters, natural disasters and terrorist attacks. Geneva: World Health Organization (Pubrights). 2023 Dec 5; 1-21.