About Jahurul Islam Medical College Hospitals
Jahurul Islam Medical College Hospitals
Articles by Jahurul Islam Medical College Hospitals
Outcome of laparoscopic varicocelectomy with mass ligation technique for symptomatic varicocele
Published on: 6th September, 2019
OCLC Number/Unique Identifier: 8251963462
Background: Varicocele therapy is a controversial issue. No single approach is adopted as the best therapeutic option. Testes get blood supply from testicular artery, cremasteric artery and artery to the vas deference. So ligation of testicular artery in the abdomen do not cause ischemia to the testis. This was already demonstrated in many studies. Classical Palomo varicocelectomy also consists of open ligation of testicular vessels in the retroperitoneum. En mass ligation of testicular vein and artery is technically easy and fast in laparoscopic varicocelectomy (LV). Chance of missing some veins are also less. Henceforth recurrence is also less. Recurrence and post-operative complications are high when only testicular vein is ligated by laparoscopy in the retroperitoneum. We wanted to see the outcome of laparoscopic varicocelectomy by mass ligation technique.
Methods: 56 patients of symptomatic varicoceles were included in the study from the outpatient services. Symptomatic varicoceles of grade 2 to grade 3 were operated from January 2012 till January 2019 over a period of 7(seven) years in Jahurul Islam Medical college Hospital. The patients were selected for dull pain and ugly veins not for infertility. All were operated by laparoscopy with en-mass ligation of testicular vein and artery in the retroperitoneum. They were followed up for a period of six months after surgery. We collected all the data in a retrospective manner.
Results: The average operation time was 27±3 minutes. Average post-operative hospital stay was 32±7 hours. There were no technical failures requiring conversion to open varicocelectomy. There was no incidence of hydrocele formation nor testicular atrophy. One patient of bilateral varicocele had 50% reduction of his varicocele. We considered this a recurrence. All other patient had complete reduction of varicocele. One patient developed hemo-peritoneum due to dislodgement of hemo-clip, which required laparotomy. He did not require any further surgery for his varicocele.
Conclusion: Laparoscopic varicocelectomy with mass ligation technique is safe, effective, less time consuming and easy to perform. Recurrence and post-operative complications are minimum. Plastic hemo-lock should be used rather than titanium heom-clip for ligation of testicular vessels. There is no incidence of testicular atrophy or any adverse effect on testis.
Lateral Pancreato-Jejunostomy in Chronic Pancreatitis: An appraisal of 32 cases
Published on: 28th January, 2020
OCLC Number/Unique Identifier: 8530264916
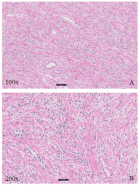
Background: Lateral Pancreaticojejunostomy (LPJ) has recognized applications in the management of Chronic Pancreatitis (CP). It is done for patients with severe pain, obstructed and dilated pancreatic duct. Ductal obstruction by stone or stricture causes rise of intraductal pressure and parenchymal ischemia. Surgical decompression of the duct and ductal drainage can achieve best pain relieve and slow the progression of the disease. We want to share our experience of removal of stones and strictures from the pancreatic duct system and drainage of the main pancreatic duct by lateral pancreatojejunostomy (LPJ) for chronic pancreatitis in a teaching institute.
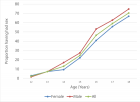
Methodology: We studied 32 cases of chronic pancreatitis operated between January 2010 and January 2017 for a period of 7 years. Patients were selected with ultrasonography, CT scan and or Magnetic Resonance Cholangio Pancreatography (MRCP). Dilatation of the main pancreatic duct by at least 7 mm proximal to the obstruction were recruited for operation. We did Roux-Y lateral pancreato-jejunostomy for patients with obstruction of the pancreatic duct due to intraductal stones or strictures. Additional distal pancreatectomy were done in two cases for stones and/or abscess in the tail area. We did one Frey’s operation for stone and fibro-calcification of the head. In all cases ductal drainage was accomplished by LPJ. We studied their post-operative pain control, complications, recurrence and improvement of exocrine and endocrine function of pancreas and mortality during this period. We followed these patients for about 2 years after surgery.
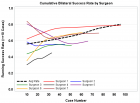
Results: We found 27 out of 32 patients got complete remission of the abdominal pain. Their progression of disease also slowed down. Ultrasonic evidence of chronic pancreatitis have improved or resolved. Ductal diameter have decreased. Two had recurrence of stones in the head and in the parenchyma within a year. 2 patients died during this follow-up period. One died three months after LPJ due to massive gangrene of the small intestine distal to LPJ and jejuno-jejunostomy and subsequent short bowel syndrome. Other one died of complications of diabetes and malabsorbtion. Pain free survival is about 84% and recurrence is 6%. Mortality during this follow up period is 6%.
Conclusion: We found that surgery, if done early, can have good remission of abdominal pain and can slow the progression of chronic pancreatitis and prevent further stone formation in majority of patients. Patient’s exocrine and endocrine function improves or remain static. Patient with chronic calcific pancreatitis and diabetes are unlikely to have favorable outcome even after decompressive surgery.
Mesh-reinforced Anterior Component Separation for Repair of Large Ventral Hernia: Ten-year Experience in Multiple Centers
Published on: 12th August, 2025
Background: Repair of a large ventral hernia is a challenge for surgeons. Component Separation Technique (CST) is a novel technique for closure of the midline with live tissues without undue tension. This can further be reinforced by a prosthesis. We wanted to see the outcome of mesh-reinforced open Anterior Component Separation (ACS) for large complex ventral hernia repair. We aimed to see the duration of surgery, hospital stay, Surgical Site Occurrence (SSO), and recurrence within the first year after surgery.Materials and methods: We analyzed data of patients operated from January 2014 to January 2024 for a period of 10 years in three centers. There were 13 patients with divarication of recti without any previous surgery. Rest 44 patients had either incisional hernia or port site hernia. All patients had defect sizes more than 8 cm. Open bilateral anterior component separations were done to achieve midline closure. Medium-pore soft Prolene mesh was used to reinforce the midline closure by an on-lay technique. Patients were followed up to 1 year after surgery to assess efficacy and complications of the procedure.Results: The average operating time was 73 ± 12 min. Hospital stay was 3 to 7 days, mean was 5.3 days. Surgical site occurrence was 14%. These include seroma formation, major wound infection, and abscess formation. There was no flap necrosis nor mesh removal. There was no recurrence within one year of follow-up after surgery. Conclusion: Open mesh Anterior Component Separation (mACS) is an easy and effective way of treating large and complex ventral hernia. Operating time is substantially less than posterior component separation. Reinforcement with mesh reduces recurrence.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."